Overview
Tennis elbow
Tennis elbow
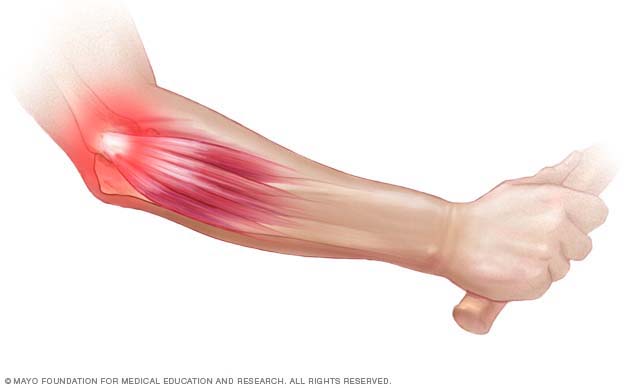
The pain of tennis elbow occurs mainly where the tough, cord-like tissues of forearm muscles, known as tendons, attach to a bony bump on the outside of the elbow. Tiny tears and longtime swelling, known as inflammation, can cause the tendon to break down. This causes the pain.
Tendinopathy is a term for any condition that affects a tendon. Tendons are cords that attach muscle to bone. Tendinopathy, which can cause pain and tenderness, is common. It is often caused by overuse or repeated movement and tends to affect certain tendons in the arm or leg.
Tendinopathy is an umbrella term for conditions affecting the tendon that include tendinitis, tendinosis and tenosynovitis:
- Tendinitis is new or sudden swelling and irritation, called inflammation, of a tendon. Often, people mistakenly call all tendon conditions by this term.
- Tendinosis is breakdown change in the tendon that occurs gradually over time.
- Tenosynovitis is inflammation of a thin layer of tissue that surrounds a tendon, called the sheath.
Tendon conditions can occur in any tendon, but they are common in the shoulders, elbows, wrists, hips, knees and heels. Most tendinopathy can be treated with rest, physical therapy and medicine to reduce pain.
Types
There are many types of tendinopathy. Common tendinopathies include:
- Achilles tendinitis. The Achilles tendon is the band of tissue that connects calf muscles at the back of the lower leg to your heel bone. Achilles tendinitis is caused by overuse or strain on the Achilles, such as when a runner increases the intensity of a running program.
- Biceps tendinopathy. Also known as bicipital tendinitis, this type of tendinopathy is irritation of the tendon that connects the biceps muscle to the shoulder joint. It's often caused by moving your arms over your head repeatedly. It also can occur at the elbow and is typically seen in people who lift heavy weights in their jobs or fitness programs.
- Calcific tendinopathy. This type of tendinopathy results from calcium deposits in a tendon. What causes calcium deposits isn't clear, but researchers believe there may be a genetic component. This condition can cause pain when moving the joint and is most common in the shoulder.
- De Quervain tenosynovitis. This painful condition, also known as Gamer's thumb, affects the tendons on the thumb side of the wrist. It is caused by long-term repeated motions of the hand or wrist. If you have de Quervain tenosynovitis, you may feel pain when you turn your wrist, grasp anything or make a fist.
- Gluteal tendinopathy. This condition is caused by inflammation of a tendon in the side of the hip. It can cause pain and tenderness in that area. It is much more common in women. You also may hear this condition referred to as greater trochanteric pain syndrome or trochanteric bursitis. The greater trochanter is part of the hip bone where muscles and tendons attach. Causes may include overuse, injury, being overweight and hormone changes.
- Golfer's elbow. Also known as medial epicondylitis, golfer's elbow causes pain where the tendons of the forearm muscles attach to the bony bump on the inside of the elbow. The pain might spread into the forearm and wrist. It's not limited to golfers, but it is often caused by repeated rotation of the forearm and wrist.
- Hamstring tendinopathy. This condition affects the tendon that connects the hamstring muscles to the "sit-bone" in the hip. It often causes pain with sitting and climbing stairs and is commonly seen in runners.
- Patellar tendinitis. This condition, also referred to as jumper's knee, is an injury to the tendon connecting the kneecap, called a patella, to the shinbone. Patellar tendinitis is most common in athletes whose sports involve frequent jumping, such as basketball and volleyball. But even people who don't take part in jumping sports can get patellar tendinitis.
- Rotator cuff injury. The rotator cuff is a group of muscles and tendons that surround the shoulder joint. Rotator cuff injuries are most often caused by wear and tear of the tendon tissue over time due to repeated overhead motions or heavy lifting. It's common in people with jobs such as carpentry or in people who play sports such as baseball or tennis. A rotator cuff injury can cause a dull ache in the shoulder that worsens at night or with reaching.
- Tennis elbow. Also known as lateral epicondylitis, tennis elbow pain can be caused by overuse of the muscles and tendons in the elbow. It's often linked to repeated motions of the wrist and arm, for example, the motions used in tennis and other similar sports.
Symptoms
Tendinopathy symptoms can vary based on the type. Symptoms tend to occur where the tendon attaches to the bone and often include:
- Pain, often described as a dull ache, especially when moving the hurt limb or joint.
- Stiffness or weakness in the affected area.
- Tenderness in the affected area.
- Mild swelling.
When to see a doctor
You can treat many cases of tendinopathy with self-care measures, such as rest, ice and pain relievers. See your healthcare professional if your symptoms don't lessen after a few days and if they get in the way of daily activities.
Causes
Tendinopathy can be caused by wear and tear on a tendon. This can happen due to overuse or naturally over time as people age and their tendons become less flexible. Most people develop tendinopathy because their jobs or hobbies involve motions they repeat over and over. Jobs such as carpentry or house painting or sports such as baseball, tennis and golf require the same motions to be repeated. Over time, this puts stress on the tendons. Some tendinopathies also can be caused by sudden injury such as a fall or accident.
How you move when doing your sport or activity can affect your risk of developing tendinopathy. Moving incorrectly can overload the tendon. Having proper form and technique is especially important when having to repeat movements for sports or a job.
Risk factors
Risk factors for developing tendinopathy include older age and having jobs or hobbies that involve doing the same motion over and over. Some medical conditions and certain medicines also may increase the risk.
Age
As people get older, their tendons become less flexible, making the tendons easier to injure.
Work
Tendinopathy is more common in certain workers, such as gardeners, carpenters and painters, whose jobs involve:
- Repeated motions, such as raking or swinging a hammer.
- Overhead motions, such as reaching up.
Activities
When you're doing physical activities, the following can increase your risk of developing a tendinopathy:
- Sudden increase in amount or difficulty of training.
- Too little recovery time after an injury or too little time to get used to the activity again after time off.
- Hard surfaces, such as concrete or gym floors.
- Poor equipment, such as old shoes or ones without good support.
- Poor posture or poor technique, such as incorrect form when playing tennis or throwing a ball.
Medical conditions and medicines
If you have certain medical conditions, such as diabetes, or take certain medicines, you can have an increased risk of tendinopathy. Medicines that may increase risk include:
- Antibiotics known as fluoroquinolones.
- Corticosteroids such as cortisone.
- Statins, used to lower cholesterol levels.
- Aromatase inhibitors, used to lower breast cancer risk.
Prevention
To lower your chance of developing a tendinopathy, follow these suggestions:
- Ease up. Avoid activities that place too much stress on the tendons, especially for long periods. If you have pain during an exercise, stop and rest.
- Mix it up. If one exercise or activity causes you pain, take a break from it and try something else. Cross-training can help you mix high-impact exercise, such as running, with low-impact exercise, such as biking or swimming.
- Improve the way you move. If you don't do an activity or exercise properly, you could be setting yourself up for problems with the tendons. Think about taking lessons or getting professional instructions when starting a new sport or using exercise equipment.
- Prepare your muscles. Strengthen muscles used in your activity or sport. For example, if you play baseball, use weights to strengthen the specific muscles you need to use. Strengthening muscles that you'll be using can help them bear the load better and lower the risk of injury.