Overview
Area commonly affected by ischemic colitis
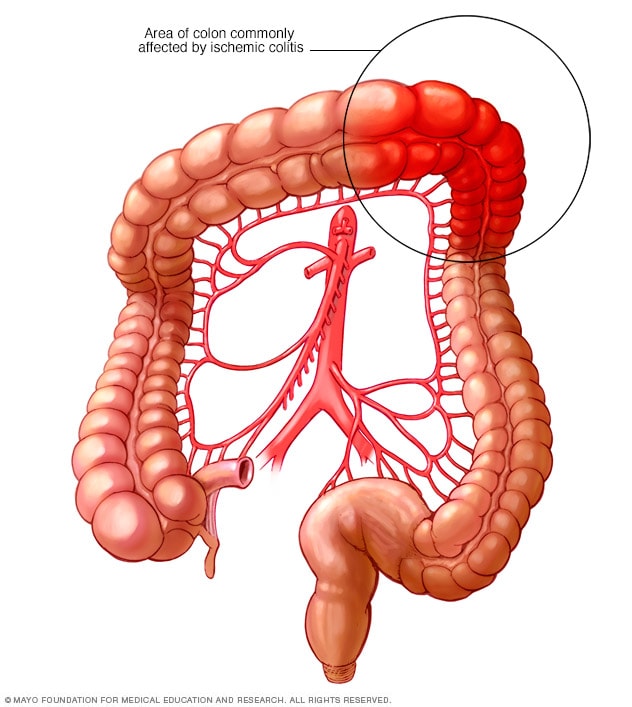
Area commonly affected by ischemic colitis
Ischemic colitis happens when blood flow to part of the large intestine, called the colon, is reduced. The condition can affect any part of the colon but is most common in the upper left segment.
Ischemic colitis happens when blood flow to part of the large intestine, called the colon, is temporarily reduced. When blood flow slows down, cells in the colon don't get enough oxygen, which may result in damage and swelling of the colon's tissues. Causes of reduced blood flow may include narrowing of the blood vessels supplying the colon or low blood pressure. Ischemic colitis is also called colonic ischemia.
Any part of the colon can be affected, but ischemic colitis most commonly causes pain on the left side of the belly area.
Ischemic colitis can be hard to diagnose because it can easily be confused with other digestive problems. You may need medicine to treat ischemic colitis or prevent infection. Or you may need surgery if your colon has been damaged. Most often, however, ischemic colitis heals on its own.
Symptoms
Symptoms of ischemic colitis can include:
- Pain, tenderness or cramping in the belly, which can happen suddenly or happen over time.
- Bright red or maroon blood in the stool or, at times, passage of blood alone without stool.
- A feeling of urgency to move the bowels.
- Diarrhea.
- Nausea.
The risk of serious complications is higher when symptoms happen on the right side of the belly. This is less commonly seen compared with left-sided colitis. People with right-sided colitis tend to have more underlying medical conditions, such as high blood pressure, atrial fibrillation and kidney disease. They more often have to undergo surgery and also have a higher risk of death.
When to see a doctor
Seek immediate medical care if you have sudden, severe pain in your belly area. Pain that makes you so uncomfortable that you can't sit still or find a comfortable position is a medical emergency.
Contact a healthcare professional if you have symptoms that worry you, such as bloody diarrhea. Early diagnosis and treatment can help prevent serious complications.
Causes
The exact cause of decreased blood flow to the colon isn't always clear. But several factors can increase the risk of ischemic colitis:
- Buildup of fatty deposits on the walls of an artery, also called atherosclerosis.
- Low blood pressure, also called hypotension, associated with dehydration, heart failure, surgery, trauma or shock.
- Bowel obstruction caused by a hernia, scar tissue or a tumor.
- Surgery involving the heart or blood vessels, or the digestive or gynecological systems.
- Medical conditions that affect the blood, including lupus, sickle cell anemia or inflammation of the blood vessels, a condition known as vasculitis.
- Cocaine or methamphetamine use.
- Colon cancer, which is rare.
The role of medicines
The use of certain medicines also can lead to ischemic colitis, though this is rare. These include:
- Some heart and migraine medicines.
- Hormone medicines, such as estrogen and birth control.
- Antibiotics.
- Pseudoephedrine.
- Opioids.
- Illicit drugs, including cocaine and methamphetamines.
- Certain medicines for irritable bowel syndrome.
- Chemotherapy medicines.
Risk factors
Risk factors for ischemic colitis include:
- Age. The condition happens mostly in adults older than age 60. Ischemic colitis that happens in a young adult may be a sign of a blood-clotting issue. It also may be due to inflammation of the blood vessels, also known as vasculitis.
- Sex. Ischemic colitis is more common in women.
- Clotting problems. Conditions that affect the way the blood clots, such as factor V Leiden or sickle cell disease, may increase the risk of ischemic colitis.
- High cholesterol, which can lead to atherosclerosis.
- Reduced blood flow, due to heart failure, low blood pressure or shock. Blood flow also can be affected by certain conditions, including diabetes or rheumatoid arthritis.
- Previous abdominal surgery. Scar tissue that forms after surgery may cause reduced blood flow.
- Heavy exercise, such as marathon running, which can lead to reduced blood flow to the colon.
- Surgery involving the heart, digestive or gynecological systems.
Complications
Ischemic colitis usually gets better on its own within 2 to 3 days. In more-serious cases, complications can include:
- Tissue death, also called gangrene, resulting from diminished blood flow.
- Hole formation, also known as perforation, in the intestine or persistent bleeding.
- Bowel obstruction, also called ischemic stricture.
Prevention
Since the cause of ischemic colitis isn't always clear, there's no certain way to prevent the disorder. Most people who have ischemic colitis recover quickly and may never have another episode.
To prevent recurrent episodes of ischemic colitis, some healthcare professionals recommend stopping any medicine that might cause the condition. Making sure to stay hydrated, especially when doing vigorous outdoor activities, is also important. This is especially true for those living in warm climates. A test for clotting problems may be recommended as well, especially if no other cause for ischemic colitis is apparent.
Nov. 07, 2024