Overview
Coarctation of the aorta
Coarctation of the aorta
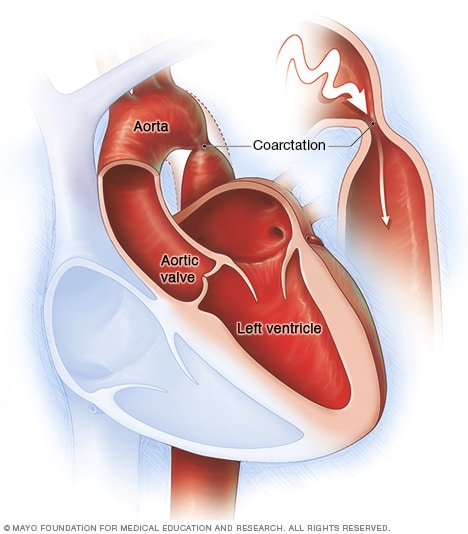
Coarctation of the aorta is a narrowing in a part of the body's main artery, called the aorta. The heart must pump more forcefully to send blood through the aorta and on to the rest of the body.
Aortic coarctation (ko-ahrk-TAY-shun) is a narrowing of a part of the body's main artery, called the aorta. The condition forces the heart to work harder to pump blood.
Coarctation of the aorta is usually present at birth. That means it is a congenital heart defect. But sometimes the condition can occur later in life.
Coarctation of the aorta often occurs along with other congenital heart defects. Treatment to fix the condition is usually successful. But regular health checkups are needed for life to watch for changes in the heart's health.
Products & Services
Symptoms
Symptoms of coarctation of the aorta depend on how much of the aorta is narrowed. Most people don't have symptoms.
Adults and older children with mild coarctation of the aorta may not have symptoms and their hearts may seem healthy.
If a baby is born with an extreme narrowing of the aorta, symptoms may be noticed shortly after birth. Symptoms of coarctation of the aorta in infants include:
- Difficulty breathing.
- Difficulty feeding.
- Heavy sweating.
- Irritability.
- Changes in skin color.
Symptoms of coarctation of the aorta later in life may include:
- Chest pain.
- High blood pressure.
- Headaches.
- Muscle weakness.
- Leg cramps.
- Cold feet.
- Nosebleeds.
Coarctation of the aorta often occurs with other heart conditions present at birth. Other symptoms depend on the specific types of congenital heart defects.
When to see a doctor
Get medical help right away for any chest pain that is extreme or can't be explained.
Also get medical help for these symptoms:
- Fainting.
- Sudden shortness of breath.
- High blood pressure that can't be explained.
These symptoms can be caused by many different health conditions. A complete health checkup is needed to learn the cause.
Causes
The cause of coarctation of the aorta is unclear. It's usually a heart problem present at birth, called a congenital heart defect. A congenital heart defect happens as the baby is growing in the womb during pregnancy. The cause is often unknown.
Rarely, coarctation of the aorta can happen later in life. Conditions or events that can narrow the aorta and cause this condition include:
- Traumatic injury.
- An extreme buildup of cholesterols and fats in the arteries, called atherosclerosis.
- A rare type of swelling and irritation of blood vessels in the heart, called Takayasu arteritis.
Risk factors
Risk factors for coarctation of the aorta include:
- Male sex.
- Some genetic conditions, such as Turner syndrome.
- Some heart conditions present at birth, called congenital heart defects.
Congenital heart defects associated with coarctation of the aorta include:
- Bicuspid aortic valve. The aortic valve is between the body's main artery and the lower left heart chamber. If the aortic valve has only two flaps, called cusps, instead of the usual three, it's called a bicuspid valve.
- Subaortic stenosis. This is a narrowing of the area below the aortic valve. It blocks blood flow from the lower left heart chamber to the aorta.
- Patent ductus arteriosus. The ductus arteriosus is a blood vessel that connects the left lung artery to the aorta. When a baby is growing in the womb, this vessel lets blood go around the lungs. Shortly after birth, the ductus arteriosus usually closes. If it stays open, the opening is called a patent ductus arteriosus.
- Holes in the heart. Some people with coarctation of the aorta also are born with a hole in the heart. If the hole is between the upper heart chambers, it is called an atrial septal defect. A hole between the lower heart chambers is called a ventricular septal defect.
- Congenital mitral valve stenosis. This is a type of heart valve disease that some people are born with. The valve between the upper and lower left heart chambers is narrowed. It's harder for blood to move through the valve.
Complications
Complications of coarctation of the aorta happen because the left lower heart chamber has to work harder to pump blood through the narrowed artery. This makes blood pressure go up in the lower left heart chamber. Also, the wall of the chamber can get thick. This condition is called ventricular hypertrophy.
Complications of coarctation of the aorta include:
- Long-term high blood pressure. Blood pressure usually drops after surgery to fix the aorta. But it may still be higher than usual.
- A weakened or bulging artery in the brain, also known as a brain aneurysm.
- Bleeding in the brain.
- A rupture or tear in the body's main artery, called an aortic dissection.
- A bulge in the wall of the body's main artery, called an aortic aneurysm.
- Coronary artery disease.
- Stroke.
Prompt treatment is needed to help prevent complications. Without treatment, coarctation of the aorta may lead to:
- Kidney failure.
- Heart failure.
- Death.
Some people have complications after treatment for coarctation of the aorta. These complications include:
- Re-narrowing of the aorta, called re-coarctation.
- Aortic aneurysm or rupture.
To prevent complications, people with coarctation of the aorta need regular health checkups for life.
Prevention
There's no known way to prevent coarctation of the aorta. Tell your healthcare team if you have a family history of heart conditions present at birth.