Diagnosis
Tests and procedures for diagnosing brain metastases include:
- Neurological exam. Your healthcare professional checks your cognition, speech, vision, hearing, balance, coordination, strength, sensation and reflexes.
-
Imaging tests. These tests make pictures of the body. Magnetic resonance imaging, also called MRI, is the main test used to help show the location and size of brain metastases. A dye may be injected through a vein in your arm during this test.
Other imaging tests may include computerized tomography, also called CT, and positron emission tomography, also called PET.
- Biopsy. Your healthcare professional may recommend a procedure to remove a sample of tissue for testing in a lab. It can be done with a needle or during surgery to remove a brain tumor.
More Information
Treatment
Treatment for brain metastases can help ease symptoms, slow tumor growth and extend life. Even with successful treatment, they may return. That's why your healthcare professional will follow you closely.
Treatments will depend on the type, size, number and location of tumors. Healthcare professionals also consider your symptoms, health and treatment goals.
Medicines to control symptoms
Medicines can help control symptoms of brain metastases and make you more comfortable. Options might include:
- Steroids. These high-dose medicines also are called corticosteroids. They may decrease swelling in the brain caused by brain metastases, helping to relieve symptoms.
- Anti-seizure drugs. These medicines may help control seizures if you have any.
Surgery
Surgery may be an option if a tumor is easily reachable and fits into your overall cancer care plan. The surgeon will remove as much tumor as possible. Surgery may help improve symptoms and help with diagnosis. It is combined with other treatments.
Brain surgery risks have improved significantly over the years. But risks may include problems with thinking, moving and speaking, as well as numbness or weakness in the face, arms or legs. Infection and bleeding are other possible risks. Risks may depend on where the tumors are in the brain.
Radiation therapy
Stereotactic radiosurgery for brain metastases
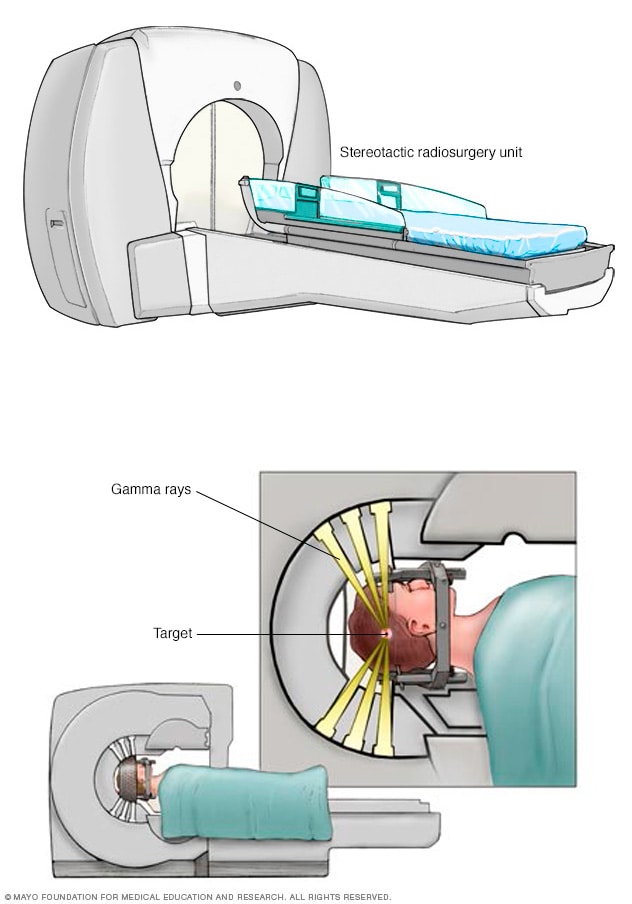
Stereotactic radiosurgery for brain metastases
During stereotactic radiation therapy, many beams of radiation are aimed at the tumor cells. Each beam isn't that powerful, but the point where all the beams meet receives a very large dose of radiation to kill tumor cells.
Radiation therapy treats cancer with powerful energy beams. The energy can come from X-rays, protons or other sources. During radiation therapy, you lie on a table while a machine moves around you. The machine directs radiation to precise points in your brain.
Treatment may include one or both of the following:
-
Whole-brain radiation. Whole-brain radiation aims beams at the entire brain to kill tumor cells. People having whole-brain radiation usually need 10 to 15 treatments over 2 to 3 weeks.
Side effects may include fatigue, nausea, skin reaction, headache and hair loss. Long-term, whole-brain radiation may cause decline in thinking and memory.
-
Stereotactic radiosurgery. Stereotactic radiosurgery is a focused radiation treatment. It also is called SRS or stereotactic body radiotherapy. SRS aims beams of radiation from many angles at the cancer.
Healthcare professionals use 3D planning to make the treatment as exact as possible and limit damage to healthy parts of the brain. Stereotactic radiosurgery may take one or a few treatments.
Side effects may include nausea, headache, seizures and dizziness. The risk of thinking and memory decline after SRS is thought to be less than with whole-brain radiation.
Healthcare professionals have made major advances understanding whole-brain radiation and stereotactic radiosurgery. They have learned how these therapies affect survival, brain function and quality of life. In deciding which radiation therapy to have, you and your healthcare professional will consider many factors. These include the number of brain metastases present, other treatments you're getting and how likely your cancer is to recur.
Medicines
Sometimes, your healthcare team may recommend medicines to control your brain metastases. Whether they may help depends on where your cancer started and your own situation. Options may include:
- Chemotherapy. Chemotherapy treats cancer with strong medicines. Many chemotherapy medicines exist. Most chemotherapy medicines are given through a vein. Some come in pill form.
- Targeted therapy. Targeted therapy for cancer is a treatment that uses medicines that attack specific chemicals in the cancer cells. By blocking these chemicals, targeted treatment can cause cancer cells to die.
- Immunotherapy. Immunotherapy for cancer is a treatment with medicine that helps the body's immune system kill cancer cells. The immune system fights off diseases by attacking germs and other cells that shouldn't be in the body. Cancer cells survive by hiding from the immune system.
Rehabilitation after treatment
Brain tumors may form in parts of the brain that control movement, speech, vision and thinking. That's why rehabilitation may need to be part of recovery. Your healthcare professional may refer you to these services:
- Physical therapy. Physical therapists can help you regain strength, coordination, and the ability to move and balance.
- Occupational therapy. Occupational therapists can help you return to your usual daily activities, such as work.
- Speech therapy. Speech pathologists can work with you if you have trouble speaking.
- Cognitive rehabilitation therapy. Healthcare professionals can help if you are having difficulty with memory loss, word recall, mood issues and attention.
Palliative care
Palliative care is a special type of health care that helps people with serious illnesses feel better. It's also called supportive care. If you have cancer, palliative care can help relieve pain and other symptoms.
Palliative care is done by a team of healthcare professionals. This can include doctors, nurses and other specially trained professionals. Their goal is to improve the quality of life for you and your family during cancer treatment.
Palliative care can happen at the same time as treatments such as surgery, radiation therapy or chemotherapy.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Alternative medicine
No alternative medicines have been found to treat brain metastases. But integrative medicine may help you cope with the stress of cancer and the side effects of cancer treatment.
Talk to your healthcare professional about your options, such as:
- Acupuncture.
- Art therapy.
- Massage.
- Meditation.
- Music therapy.
- Physical activity.
- Relaxation exercises.
- Yoga.
- Nutrition.
Coping and support
Mayo Clinic Connect: Brain tumors
Mayo Clinic Connect: Cancer
Coping with brain metastases involves accepting the news that your cancer has spread beyond its original site.
Cancer that has spread can be difficult to cure. People with a single brain metastasis have a better chance of long-term survival than do people with multiple metastatic tumors. Your healthcare team will work to reduce your pain and help you continue your daily activities.
With time you'll find ways to cope with the stress and uncertainty of cancer. Until then, you may find that it helps to:
- Learn about brain metastases. Ask your healthcare professional for details of your cancer. Ask about the type, treatment options and your prognosis. Ask for good sources of up-to-date information.
- Be aware of possible limits on driving. Ask your healthcare professional if it's OK for you to drive. The answer may depend on if your neurological exam shows that your judgment and reflexes have not been affected and whether you have seizures.
- Express your feelings. Find an activity that allows you to write or talk about your emotions. That may include writing in a journal, talking to a friend, counselor or chaplain, or joining a support group. Ask your healthcare professional about support groups in your area.
- Come to terms with your illness. If treatment isn't helping, you and your family may want to talk with your healthcare team about end-of-life care options, such as hospice.
Preparing for your appointment
Make an appointment with your healthcare professional if you have any symptoms that worry you. Tell them if you've been treated for cancer before, even if it was many years ago.
If you're diagnosed with brain metastases, you'll be referred to one or more of the following healthcare professionals:
- A neuro-oncologist, who specializes in brain metastases.
- A neurologist, who treats disorders of the nervous system.
- A radiation oncologist, who treats brain tumors with radiation.
- A neurosurgeon, who performs surgery on brain tumors.
Appointments can be brief, and there's a lot to discuss. It's a good idea to be prepared. Here's how to help get ready and what to expect:
What you can do
- Be aware of any pre-appointment rules. When you make the appointment, ask if there's anything you need to do in advance, such as change your diet.
- Write down your symptoms, even those that may not seem related to why you scheduled the appointment. Note how long you've had these symptoms and what makes them worse or better.
- List key personal information, including any major stresses or recent life changes.
- Make a list of all medications, vitamins or supplements that you're taking. Include doses.
- Consider taking a family member or friend along. Sometimes it can be difficult to remember all the information provided during an appointment. Someone who comes with you may remember details you missed or forgot.
- Write down questions to ask your healthcare professional.
Writing a list of questions can help you make the most of your time with your healthcare professional. For brain metastases, some basic questions to ask include:
- What's the most likely cause of my symptoms?
- Are there other possible causes for my symptoms?
- What kinds of tests do I need?
- What treatments are available, and which do you recommend?
- What are the possible side effects of each treatment?
- How will treatment affect my daily life?
- How long will the treatment last?
- What's my prognosis?
- What experimental treatments or clinical trials are available to me?
- I have these other health conditions. How will those affect my treatment?
- Is there a generic alternative to the medicine you're prescribing me?
- Do you have any brochures or other printed material that I can take with me? What websites do you recommend?
- If you had a friend or loved one in my situation, what advice would you give them?
What to expect from your doctor
Your healthcare professional is likely to ask you several questions, including:
- When did you first experience symptoms?
- Are your symptoms continuous or do they come and go?
- How severe are your symptoms?
- What, if anything, helps improve your symptoms?
- Does anything make your symptoms worse?
Nov. 20, 2024