April 10, 2024
 المشيمات الطبيعية وغير الطبيعية
المشيمات الطبيعية وغير الطبيعية
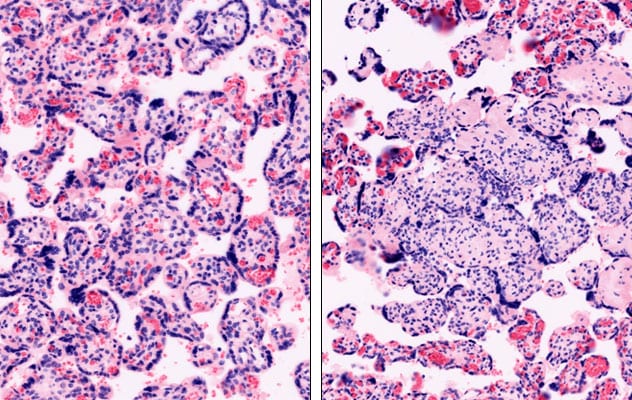
تظهر الصورة على اليسار مشيمة طبيعية، بينما تظهر الصورة على اليمين مشيمة ملتهبة.
A Mayo Clinic study assessing placental pathology reports after fetal surgery for congenital defect repair found that the interventions did not increase abnormal placental findings. The findings were published in Prenatal Diagnosis in 2023. The investigators observed no increased inflammatory pathologies in placentas of women who had the surgery compared with those who did not.
"We undertook this study because while we know fetal surgery is incredible — it greatly improves infant outcomes after in utero congenital defect repair — we didn't know how the placenta responded," says Elizabeth Ann L. Enninga, Ph.D., an immunologist at Mayo Clinic's campus in Minnesota and a study author. "These findings are important to fetal surgery because they demonstrate no impact on placental outcomes and support surgery in utero to repair certain congenital defects."
Study design and findings
In this case-control study, investigators divided women into three groups: 22 women who had fetal surgery at 22 to 28 weeks' gestation, 13 women with an indication for fetal surgery who did not have prenatal intervention, and 36 gestational age-matched controls.
The investigators observed no placental differences in inflammation or vascular defects among groups. They discovered that any postpartum placental pathologies present were related to gestational age and not surgical intervention, says Dr. Enninga.
This result came as a surprise.
"I thought we'd see an increase in inflammatory pathologies," Dr. Enninga says. "The fact that we didn't wasn't my first hypothesis, but I'm happy it turned out this way, as our goal is healthy moms and babies."
Mauro H. Schenone, M.D., a fetal surgeon at Mayo Clinic in Minnesota and study author, calls the findings reassuring to patients undergoing fetal surgery, as the findings suggest that surgery does not significantly increase placental histologic inflammatory changes. For counseling patients regarding fetal surgery, he indicates that this study provides further risk-benefit information to discuss.
"This means fetal surgery isn't as inflammatory to the intrauterine environment as some thought, at least at the placental level," says Dr. Schenone. "Our hypothesis was that fetal surgery would increase placental inflammation. Yet what we found was the opposite."
In the fetal surgery field, Dr. Enninga says this study is the largest of its kind and most convincing regarding post-fetal surgery placental findings. She notes that other studies included only two or three placentas.
While the Mayo Clinic study is a larger fetal surgery study, its smaller numbers in broader medical research prompt the authors to state that these findings offer modest patient, physician and institutional review board reassurance that electing fetal surgery is unlikely to affect placental structure and function.
"We can't definitely say there's no inflammation with these numbers alone, but there were no inflammatory indications in the placentas we studied," says Dr. Enninga.
The next step in this research is a multisite study with larger numbers to confirm the Mayo Clinic study's findings, says Dr. Schenone, indicating that a single-institution study may lack subtle-difference detection power.
Inflammation: A factor for good or ill
Dr. Enninga is quick to mention that inflammation is common and can work for good or ill and that any surgery can lead to inflammation. She notes that when inflammation becomes chronic and the immune system cannot control it, disease develops.
For a fetus, data indicate that inflammatory exposure in utero can have negative neurological development effects later in life, Dr. Enninga says, usually presenting as young children who miss developmental milestones. Immunologists reviewing the placenta in such cases have found significant pathology. Placental inflammation can become recurrent and negatively impact the next pregnancy, she says.
"If the placenta is bad — negatively affected by inflammation — the fetus will have a harder time developing as it should," she continues.
Fetal surgery risks and benefits
Despite in utero surgery fetal benefits, Dr. Enninga notes that the mother does not directly benefit from it. In fact, fetal surgery comes with maternal risks and may or may not help the fetus, say Drs. Enninga and Schenone.
"From a fetal perspective, in utero surgery increases risk of prematurity and its consequences," Dr. Schenone adds.
When asked about fetal surgery's benefits, Dr. Schenone says it potentially can be a lifesaving intervention in a situation such as early gestational age severe fetal anemia or advanced-stage twin-twin syndrome, in which mortality rates range from 70% to 100% without intervention. More-recent evidence shows that surgery in utero to block the trachea and increase lung pressure can promote prenatal lung growth and increase survival for fetuses with congenital diaphragmatic hernia. Beyond life-threatening situations, repairing other conditions in utero can benefit fetal development. An example is spina bifida, in which the neural tube does not close completely.
"With spina bifida, you have exposed fetal neural elements, hindbrain herniation and in many cases ventriculomegaly," says Dr. Schenone. "In utero spina bifida repair helps prevent or minimize further prenatal damage and leads to improved postnatal outcomes."
Preterm birth: Fetal surgery's Achilles heel
Dr. Enninga says one fetal surgery challenge is its association with preterm delivery, which can be inflammation mediated.
The risk and degree of prematurity greatly depends on fetal surgery's type and timing. Uterine and amniotic membrane trauma have a key role, Dr. Schenone adds.
Dr. Enninga says the Mayo Clinic investigative team now is researching maternal inflammation, hypothesizing that maternal blood factors may help predict preterm birth following surgery.
Meanwhile, she says, "everyone wants more fetal surgery data" and calls on medical centers to work together and share results.
Mayo Clinic's fetal surgery
While few U.S. and worldwide medical centers offer fetal surgery, Mayo Clinic is committed to continuing to build its in utero intervention practice and fetal surgery research. Toward this end, another fetal surgeon, Kholoud Arab, M.B.B.S., has joined the practice.
"At Mayo Clinic, there are real options for fetuses with conditions such as spina bifida or congenital diaphragmatic hernia," says Dr. Enninga. "Fetal surgery gives the organ or tissue more time to develop appropriately long-term."
Fetuses have an incredible ability to repair and regenerate, she says. Thus, fetal surgery can be crucial for best outcomes. She also notes that fetuses with spina bifida repaired in utero experience fewer complications than they do with postpartum surgery when infants cannot heal as easily.
Dr. Enninga says although fetal surgery is medically complex, Mayo Clinic has excellent infrastructure for its program, with expertise, support staff and capability to affordably house pregnant patients and their families through a community nonprofit.
If you would like to refer a pregnant patient for fetal surgery evaluation, Dr. Schenone encourages considering Mayo Clinic. He says he enjoys being a Mayo Clinic fetal surgeon due to the medical center's multidisciplinary nature, with many specialists under one roof with whom he can consult. Beyond meeting with these specialists presurgically, the specialist will at times partner with Dr. Schenone in fetal surgery.
For more information
Cardenas MC, et al. Fetal surgery is not associated with increased inflammatory placental pathology. Prenatal Diagnosis. 2023;43:382.
Refer a patient to Mayo Clinic.