Sept. 23, 2022
神经瘤
自体游离肌肉移植物
自体游离肌肉移植物
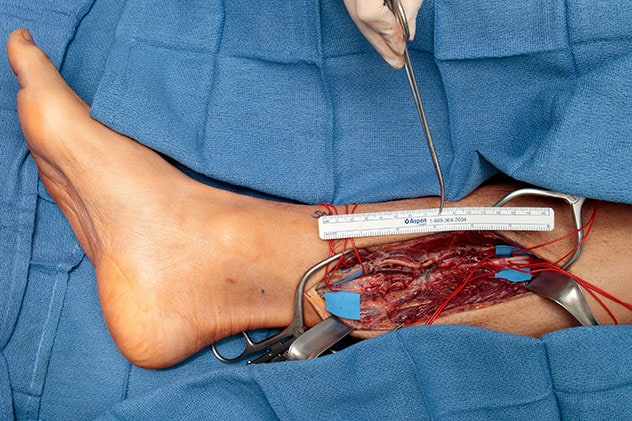
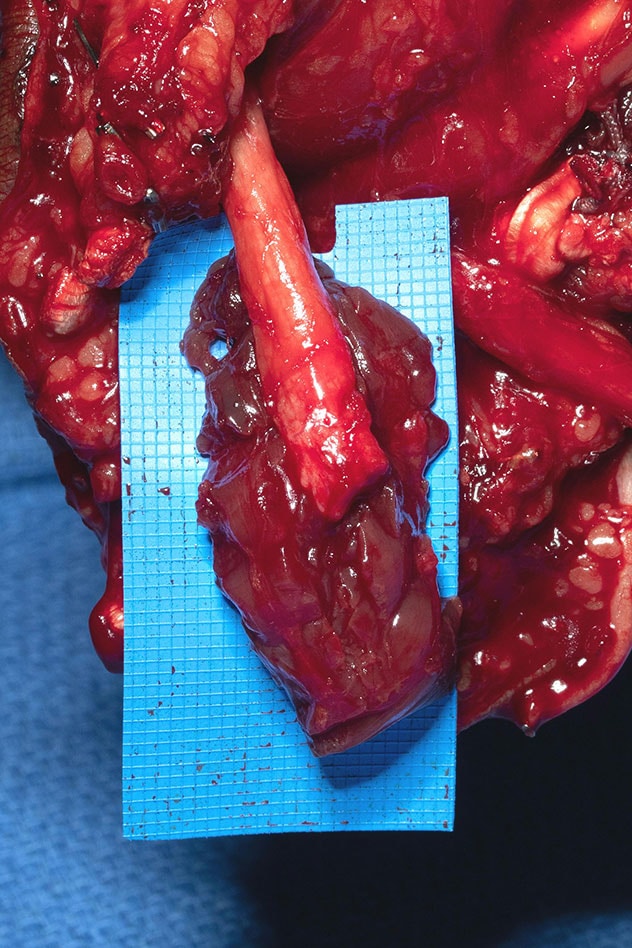
神经切除术(一种神经瘤切除手术)后,显示了通过显微外科手术进行固定之前游离肌肉移植物的放置情况
Mayo Clinic is employing a new method of pain prevention as part of limb amputation, heading off post-amputation morbidity from the formation of neuromas, which contribute to residual limb pain (RLP) and phantom limb pain (PLP). Until recently, traditional interventions for post-amputation neuromas have been unsuccessful: Neuroma recurrence rates were high.
The new method, regenerative peripheral nerve interface (RPNI), has been studied both preclinically and clinically. It prophylactically reduces potentially symptomatic neuromas through autologous free muscle grafts, often from the amputated limb, implanting the ends of transected nerves into the graft and supplying regenerating axons, reinnervating end organs and creating new neuromuscular junctions.
"RPNI is active prevention of neuroma," says Shelley S. Noland, M.D., a hand and peripheral nerve surgeon at Mayo Clinic's campus in Arizona, and a major user of the RPNI technique. "Placing the nerve endings into muscle graft tissue gives the nerves somewhere to go and something to do."
Although RPNI ideally is performed at the time of amputation, Dr. Noland explains that RPNI can be performed later, if a neuroma forms post-amputation. The surgeon resects the neuroma and performs the RPNI procedure, solving the anatomical issue. She notes if RPNI is performed after a neuroma forms, however, it can take significant time for the brain to stop registering pain, despite the procedure's removing its source.
In the U.S., the most common type of amputation involves the lower extremity, says Dr. Noland. According to a study by Kathryn Ziegler-Graham, Ph.D., and colleagues published in a 2008 issue of Archives of Physical Medicine and Rehabilitation, as of 2005, 1 out of 190 U.S. individuals — 1.6 million people — had experienced limb amputation.
A projection for U.S. amputation volume for the year 2050 is 3.6 million individuals, barring a significant decrease in dysvascular disease — a condition with rising incidence currently — according to this study. Post-surgically, up to 80% of patients experience PLP, according to a 2021 publication in Pain Reports by Joachim Erlenwein and colleagues. Of all amputees, 50% experience residual limb pain, according to Thomas Buchheit, M.D., and colleagues' 2016 publication in Pain Medicine.
"Pain is a major issue post-amputation," Dr. Noland says. "Neuromas are incredibly painful. They lead to chronic pain and a terrible cascade of issues."
In a study published in a 2017 issue of Prosthetics and Orthotics International by Richa Sinha and colleagues, investigators found pain from post-amputation neuroma is associated with decreased quality of life.
Dr. Noland says neuromas often become superficial, and patients can identify their precise locations and palpate them.
"Pain from a neuroma can be so intense that patients are less able to participate in daily life activities and may give up on prosthetic use," says Dr. Noland.
"It's hard to function if your prosthetic is pushing on a neuroma," she explains. "You just can't do it."
Due to potential for significant morbidity post-amputation, Dr. Noland believes it's important for surgeons who amputate limbs to mitigate pain during the amputation or by treating symptomatic neuromas post-amputation.
Active, effective prevention versus inconsistent, passive prevention
The traditional method of deterring neuroma formation involved attempting to bury the nerve ends at the amputation site, effectively placing them away from the surface. However, Dr. Noland indicates high failure rates with these techniques, primarily because the buried nerves did not stay in place.
Physicians developed RPNI because former amputation techniques were inconsistently successful for pain prevention and did not offer the severed nerves a function, which all nerves instinctively seek.
"The old techniques didn't give the nerves at the amputation site anywhere to go or anything to do," Dr. Noland says. "A nerve will try to grow proximal to distal, and when it has nowhere to go, it makes a big hard ball of nerve scar. This was a passive approach to prevent neuroma, where RPNI is active prevention of neuroma."
Additionally, RPNI is intended to be a long-term solution to post-amputation pain from neuroma formation. Dr. Noland reports she has not seen a neuroma develop after RPNI. She notes, however, that while there is some one-year follow-up for the procedure, clinical investigators are still working on determining long-term outcomes from RPNI as the procedure evolves.
Safety and feasibility for many orthopedic surgeons
According to a 2021 article published in Annals of Vascular Surgery, RPNI has proved to be safe. In addition, unlike other challenging-to-duplicate, extremely complex orthopedic surgical techniques, it is highly replicable by a wide spectrum of surgeons in the field.
Availability of RPNI
Dr. Noland says RPNI is not commonplace in the U.S. currently, and she believes the technique's potential is not yet widely known in the orthopedic community. To spread the word about RPNI, she is attempting to provide education for orthopedic surgeons, starting with home-base education about sarcoma cases at Mayo Clinic's campus in Arizona.
The technique requires both nerve and microsurgical expertise, a combination she says is far more common in academic medicine.
For more information
Ziegler-Graham K, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Archives of Physical Medicine and Rehabilitation. 2008;89:422.
Erlenwein J, et al. Clinical updates on phantom limb pain. Pain Reports. 2021;6:e888.
Buchheit T, et al. Pain phenotypes and associated clinical risk factors following traumatic amputation: Results from veterans integrated pain evaluation research (VIPER). Pain Medicine. 2016;17:149.
Sinha R, et al. Factors affecting quality of life in lower limb amputees. Prosthetics and Orthotics International. 2017;35:90.
Kubiak CA. Decreasing postamputation pain with the regenerative peripheral nerve interface (RPNI). Annals of Vascular Surgery. 2021:79;421.
Refer a patient to Mayo Clinic.