Aug. 06, 2021
病理性髋臼骨折和股骨头上移

病理性髋臼骨折和股骨头上移
一名新诊断为转移性肺癌的 56 岁男性,前来妙佑医疗国际就诊时,其右髋关节疼痛严重,导致无法行走,右髋关节前后位 X 光片显示病理性髋臼骨折和股骨头上移至髋臼缺损处。
病理性髋臼骨折伴后壁和后柱缺失

病理性髋臼骨折伴后壁和后柱缺失
一名 56 岁男性新诊断为转移性肺癌,他在妙佑医疗国际就诊时右髋关节疼痛严重,无法行走,骨盆闭孔斜位 X 线显示病理性髋臼骨折,后壁和后柱缺失,右髋关节后半脱位。
上髋臼和后髋臼骨量丢失
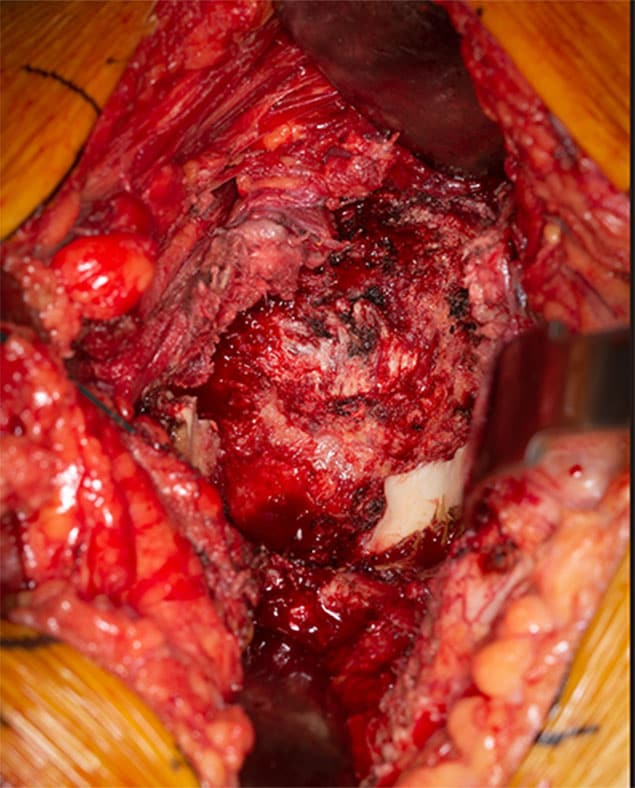
上髋臼和后髋臼骨量丢失
一名 56 岁男性新诊断为转移性肺癌,他在妙佑医疗国际就诊时右髋关节疼痛严重,无法行走,术中照片显示严重的上髋臼和后髋臼骨量丢失。只有髋臼的下侧类似于天然解剖结构。
最终重建
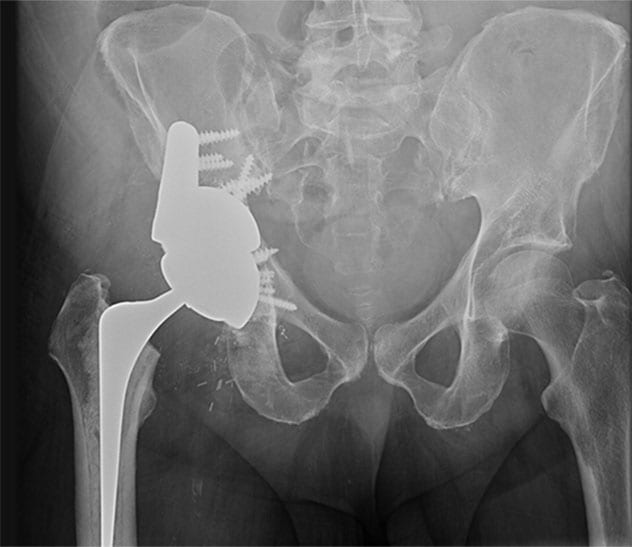
最终重建
一名 56 岁男性新诊断为转移性肺癌,他在妙佑医疗国际就诊时右髋关节疼痛严重,无法行走,术后 X 线检查显示了最终重建。在髋臼上部缺损处放置一个高度多孔钽金属加强块,然后插入一个高度多孔的钽金属修复壳,使加强块与剩余的耻骨和坐骨之间形成压合。在完整髂骨上附加固定一个额外的支撑垫块,它也由高度多孔的钽金属制成。由于计划在未来进行放射治疗,因此还采用了骨水泥柄全髋关节成形术。术后,患者疼痛显著缓解,并恢复了行走能力。
Joint reconstruction is particularly challenging in the setting of complex bony defects or radiation therapy. Mayo Clinic routinely uses 3D-printed models to optimize surgical outcomes for individual patients.
"This technology allows us to re-create a patient's bony defects and surgically correct them to restore joint function," says Cory G. Couch, M.D., an orthopedic surgeon at Mayo Clinic in Rochester, Minnesota, with fellowship training in orthopedic oncology and joint reconstruction. "We are able to model and fill in even very large bony defects created by tumors and tumor resections."
Mayo Clinic has the largest point-of-care additive manufacturing facility in the United States, staffed by radiologists and biomedical engineers. "They work in close conjunction with us," Dr. Couch says. "Complex joint reconstructions require multidisciplinary care from imaging experts and from radiation and medical oncologists, as well as orthopedic surgeons."
The 3D-printing technology is used in complex reconstructions of the knee, hip and pelvis for individuals with sarcoma or metastatic cancer. The technology also facilitates complex joint replacements associated with infection or the failure of a previous replacement joint.
The models are created using individual patients' CT scans or MRI or both and sterilizable materials. "In the operating room, we have the model on the table right next to the patient. That helps us to identify optimal implant placement or screw fixation," Dr. Couch says.
Arthroplasty and cancer care
Mayo Clinic commonly treats patients with bony defects due to cancer. Radiation and medical oncologists meet regularly with orthopedic surgeons to discuss patients and plan treatment. Surgical reconstruction of the hip or knee may precede or follow radiation treatment.
"We typically make these decisions based on the tumor type and location, but sometimes on a case-by-case basis," Dr. Couch says. "Sometimes having chemotherapy or radiation therapy upfront will reduce the size of the tumor, facilitate removal and optimize the maintenance of function."
Historically, patients having total hip arthroplasty after pelvic radiation experienced high rates of implant loosening when traditional uncemented acetabular components were used. But Mayo Clinic orthopedic researchers have found that 100% of modern, porous titanium components remained radiologically well fixed 10 years after implantation in patients having total hip arthroplasty after pelvic radiation. As described in the Journal of Arthroplasty, the mean overall pelvic radiation dose for the 33 patients in the study exceeded the radiation threshold for dose-related bone effects.
A separate study, described in The Journal of Bone and Joint Surgery, found that for patients with periacetabular metastatic disease, acetabular reconstruction using highly porous tantalum components provided a more durable construction and fewer complications compared with procedures using the cemented technique.
"Advances in medical care and radiotherapy mean that more cancer patients are living longer," Dr. Couch says. "Restoring patients' joints allows them to return to walking soon after surgery. The goal is for these patients to spend the remainder of their lives doing the things they want to do, relatively pain-free."
For more information
Wellings EP, et al. Contemporary porous titanium acetabular components for total hip arthroplasty after pelvic radiation. Journal of Arthroplasty. 2021;36:1714.
Houdek MT, et al. Comparison of porous tantalum acetabular implants and Harrington reconstruction for metastatic disease of the acetabulum. The Journal of Bone and Joint Surgery. 2020;102:1239.