Sept. 14, 2019
To determine whether findings seen in international studies are applicable to a U.S. cohort, John J. Chen, M.D., Ph.D., and a research team with Ophthalmology at Mayo Clinic in Rochester, Minnesota, evaluated the risk of stroke after central retinal artery occlusion (CRAO) in patients at Mayo Clinic.
急性视网膜中央动脉阻塞
急性视网膜中央动脉阻塞
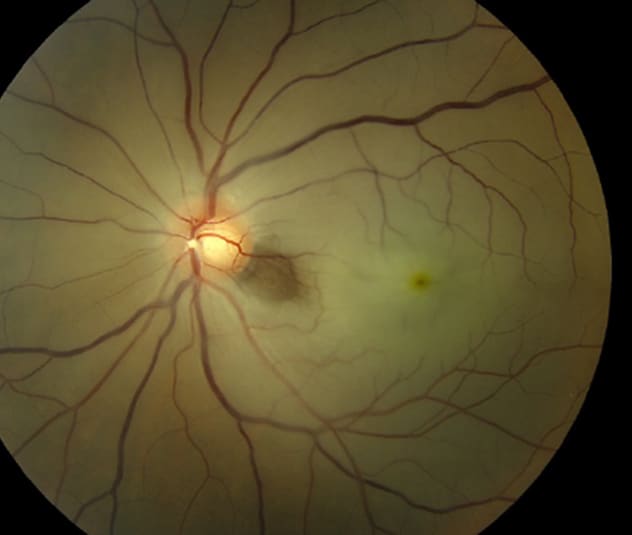
左眼眼底照片显示视网膜中央动脉阻塞伴视网膜白化、樱桃红斑以及从视盘出来的小动脉内出现斑块。
Occlusion of the central retinal artery and its branches that perfuse the inner retina can produce acute vision loss in the affected eye. The incidence of CRAO has been estimated at 1 to 2 per 100,000 people a year, and 80% of patients with CRAO have profound vision loss with a final visual acuity of 20/400 or worse.
In addition to debilitating vision loss, however, studies from Taiwan and Korea, published in the American Journal of Ophthalmology in 2012 and Ophthalmology in 2015, respectively, suggest that retinal artery occlusions are associated with an increased risk of ischemic stroke. "Since these articles were published, content experts have proposed that retinal artery occlusions are an emergency and recommend cerebrovascular evaluation within 24 hours," says Dr. Chen. "Our goal was to provide evidence from the U.S. to help guide the discussion on how quickly a comprehensive cerebrovascular evaluation and work-up should take place in patients with CRAO."
Study results were published in Mayo Clinic Proceedings in 2019.
Researchers reviewed charts for patients older than 18 years with a confirmed new diagnosis of CRAO from Jan. 1, 2001, through Sept. 9, 2016, at Mayo Clinic sites in Rochester, Minnesota; Jacksonville, Florida; and Phoenix/Scottsdale, Arizona. Information gathered included:
- Patient sex
- CRAO laterality
- Patient age at the time of diagnosis
- Cause of CRAO
- Ischemic stroke within 15 days before or after CRAO
- Transient ischemic attack (TIA) within 15 days before or after CRAO
- Amaurosis fugax within 15 days before or after CRAO
"We took care to determine the time course of stroke and CRAO, including noting when stroke and CRAO occurred on the same day," says Dr. Chen. "Peri-CRAO stroke included stroke within 15 days before CRAO, simultaneously with CRAO, or 15 days after CRAO. In patients whose work-up included MRI, we recorded asymptomatic diffusion restriction, indicating clinically silent cerebral ischemia. Evidence of old or chronic cerebral ischemia on MRI was also noted."
Ultimately, 300 patients with CRAO were included in the study cohort. The median age at the time of CRAO was 72 years, and 158 of the patients were male. Overall, 16 patients (5.3%) had symptomatic ischemic stroke around the time of CRAO, with seven strokes (2.3%) occurring 15 days before CRAO, four (1.3%) occurring simultaneously with CRAO, and five (1.7%) occurring after CRAO.
In addition, 25 of 110 patients (22.7%) had either symptomatic stroke or asymptomatic diffusion restriction among patients who underwent MRI around the time of CRAO, which further highlights the connection between CRAO and stroke.
Dr. Chen notes: "The two most common causes of CRAO were embolic and unknown, with thrombotic, vasculitic, surgical complications and central retinal vein occlusion-induced CRAO each causing a smaller number of CRAOs. Of the patients with embolic CRAO, 7% had a peri-CRAO stroke compared with 1.3% of patients with an unknown cause of CRAO. The overall peri-CRAO stroke risk was similar to that of previous international reports on the risk of stroke and CRAO."
In 2017, research published in Ophthalmology Retina retrospectively reviewed a cohort of patients with CRAO in the U.S. and found a 7% risk of TIA or stroke before or after CRAO, with 1% occurring within three months after CRAO. "In conjunction with these studies, our study supports that there is a clear increased risk of stroke around the time of CRAO, especially if an embolic etiology of CRAO is diagnosed," says Dr. Chen. "This study provides further evidence of the increased risk of ischemic stroke, including asymptomatic cerebral infarctions, in the peri-CRAO period.
"Therefore, if a patient is diagnosed with an acute CRAO, an urgent cerebrovascular work-up is required, with an emphasis on carotid imaging."
For more information
Chang YS, et al. Retinal artery occlusion and the 3-year risk of stroke in Taiwan: A nationwide population-based study. American Journal of Ophthalmology. 2012;154:645.
Park SJ, et al. Risk and risk periods for stroke and acute myocardial infarction in patients with central retinal artery occlusion. Ophthalmology. 2015;122:2336.
Chodnicki KD, et al. Stroke risk before and after central retinal artery occlusion in a US cohort. Mayo Clinic Proceedings. 2019;94:236.
Hayreh SS, et al. Ocular arterial occlusive disorders and carotid artery disease. Ophthalmology Retina. 2017;1:12.