July 27, 2024
A Mayo Clinic study found that a multidisciplinary surgical approach guided by modified Mohs surgery achieved better recurrence-free survival for patients with female extramammary Paget's disease (EMPD) when compared with traditional wide local excision (WLE). The findings were recently published in the American Journal of Obstetrics and Gynecology (AJOG).
Margin-controlled surgery, including modified Mohs surgery, has previously been shown to improve outcomes in male genital EMPD. The investigators embarked on this study to see if this finding held true for female anatomy.
"This is a very frustrating disease for patients and healthcare professionals," says Bill Cliby, M.D., a gynecologic oncologist at Mayo Clinic in Minnesota and AJOG paper co-author.
The Mayo Clinic investigators had observed frequent EMPD recurrences following the traditional surgical approach; thus, they sought a more effective surgical method, according to Kelly H. Bruce, M.D., M.S. Dr. Bruce is the first author of this study and a gynecologic oncology fellow at Mayo Clinic in Minnesota who completed her master's thesis on EMPD.
"Female genital Paget's disease is really challenging," says Jamie N. Bakkum-Gamez, M.D., a gynecologic oncologist at Mayo Clinic in Minnesota and AJOG paper co-author. "For patients, it can be debilitating — they can become hopeless due to this disease's recurring nature."
Urologists see EMPD in patients with male anatomy, and gynecologists see patients with female anatomy. Dr. Bakkum-Gamez says this division can lead to treatment differences for similar conditions.
"Mayo Clinic urologists had partnered with dermatologic surgeons for some time when we began this study in gynecologic oncology," says Dr. Bakkum-Gamez. "We heard about Mohs surgery's success in male anatomy, resulting in fewer recurrences in men than in women. This is a gender inequity. We wanted to study this procedure in women with Paget's to give them the best possible treatment."
Study details
 外阴病变
外阴病变
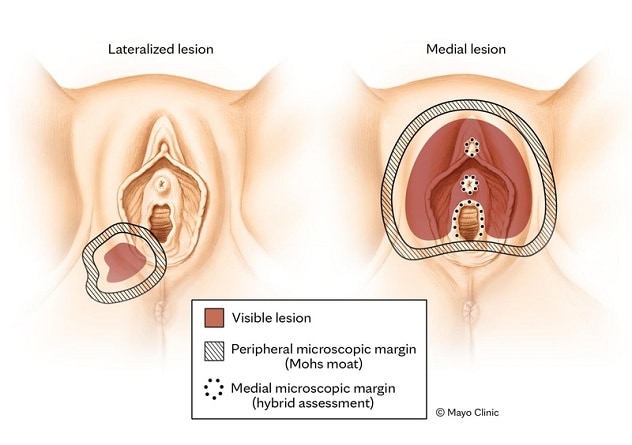
生殖器皮肤癌偏侧和正中外阴病变的位置。为在《妇科肿瘤学》上发表而创建的资产。
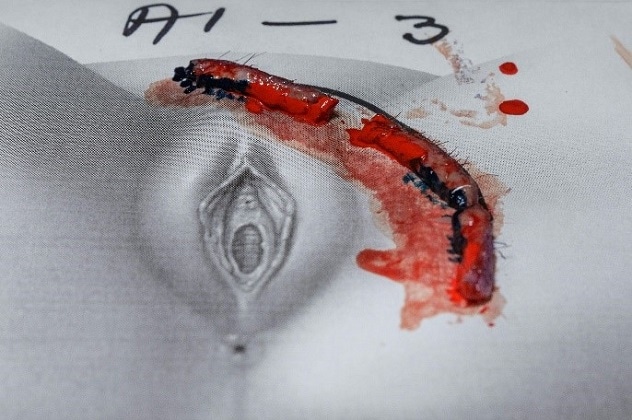 墨染切缘
墨染切缘
EMPD 莫氏手术对切缘进行了墨染。
 切除 moat
切除 moat
改良莫氏手术使用含细胞角蛋白 7 染色的 moat 技术清除外周疾病边缘。
The investigators conducting this prospective, observational study compared surgical and oncologic outcomes for two patient groups with EMPD:
- Patients who underwent traditional WLE for vulvar or perianal Paget's disease (retrospective comparison group).
- Patients with the same disease who underwent a multidisciplinary surgical approach guided by Mohs surgery (prospective pilot group).
Patients who underwent WLE experienced a three-year recurrence-free survival of 65.9%. In contrast, patients who underwent Mohs surgery experienced a 93.3% recurrence-free survival in the same duration.
The multidisciplinary protocol included outpatient scouting biopsies and modified Mohs surgery followed by surgical excision with wound closure under general anesthesia. Modified Mohs surgery cleared peripheral disease margins using a moat technique with cytokeratin 7 staining. A hybrid of Mohs surgery and intraoperative frozen sections examined medial disease margins in structures such as the clitoris, urethra, vagina and anus. The two cohorts had similar maximum surgical specimen diameters: 9.5 cm for WLE and 11.3 cm for Mohs. However, the investigators discovered that patients who had Mohs surgery required more-complex reconstructive surgeries: 66.7% of patients who had Mohs surgery needed plastic surgery reconstruction compared with 30.2% of patients who had WLE.
Mohs surgery challenges
While margin control using Mohs surgery significantly improved short-term, recurrence-free survival following EMPD excision, this procedure is technically challenging and time intensive. Modified Mohs surgery involves excision of small strips of skin one at a time followed by microscopic examination of each for the presence of cancer. This process continues until the dermatologic surgeon encounters a noncancerous strip. Studies have shown that portions of an EMPD lesion are not visible to the naked eye, thus this microscopic examination is critical. Mohs surgery allows the surgeons to ensure cancer-free excisional margins and may spare surgery to sensitive areas like the clitoris if that skin is cancer-free. The approach becomes complex when EMPD directly involves sensitive structures such as the clitoris, urethra, vagina and anus.
"There is a fine balance between aggressiveness versus sacrificing some margin to avoid destroying essential structures," says Dr. Cliby.
The investigators indicate that Mohs surgery is highly effective for lesions that do not involve critical perineal structures but will require further optimization for lesions that involve these sensitive structures, such as urethra, vagina and anus.
How Mayo Clinic can help patients with extramammary Paget's disease
While EMPD is rare, Dr. Cliby indicates he and his colleagues see numerous patients with this disease, as Mayo Clinic is a tertiary referral center.
Mayo Clinic gynecologic oncologists collaborate with dermatologic, colorectal, urologic and plastic surgeons for treatment. Mayo Clinic dermatologic surgeons are experts in Mohs surgery, even in delicate female anatomy, and Mayo Clinic plastic surgeons aptly address female functional and sexual needs. Colorectal surgeons and urologists assist when the disease involves the anus or urethra. Dr. Bruce says effective margin-controlled surgery requires a medical center such as Mayo Clinic with specialized, collaborative care. She recommends a prompt referral for vulvar EMPD, and the team emphasizes that EMPD requires strong preoperative counseling, as patients' wishes and needs vary widely.
This multidisciplinary team also treats patients with female genital Paget's disease who have undergone WLE at other medical centers and have residual or recurrent disease and suggests referring patients with this status.
About this cancer
EMPD is rare. Invasive and metastatic EMPD is rarer still and can be deadly, according to Dr. Bakkum-Gamez.
She also says even experts may disagree on EMPD terminology.
"It can be hard for patients to make decisions regarding Paget's disease," Dr. Bakkum-Gamez says. "One healthcare professional might say Paget's is not a true cancer and will not take your life. Many healthcare professionals treat this disease as though it were not dangerous if they don't have all the risk information. Yet, another healthcare professional might call it cancer."
She confirms that at Mayo Clinic, Paget's disease is considered a cancer.
Dr. Bakkum-Gamez says dermatologists may discover this slow-growing cancer at a patient's skin check. Primary care physicians and general gynecologists also find EMPD during pelvic exams. EMPD often occurs in anatomy with apocrine sweat glands, which exist in large quantity in the pelvic region.
This disease often presents with substantial itching, though the patient may have multiple symptoms.
"Extramammary Paget's disease has a broad range of symptoms," says Dr. Bruce. "Some patients are miserable if the Paget's affects the vaginal canal."
It is not unusual for patients to feel their disease is minimized en route to an EMPD diagnosis. Dr. Cliby says most women are initially treated empirically with antiyeast creams and other topical medications. This approach of empiric treatment often delays diagnosis by months to years, and Dr. Bruce recommends prompt vulvar skin biopsy for patients who do not respond to empiric treatment.
A workup for this disease includes a comprehensive cancer screening, including mammography, colonoscopy, urine cytology and screening around the area where skin symptoms are present.
For more information
Bruce KH, et al. Mohs surgery for female genital Paget's disease: A prospective observational trial. American Journal of Obstetrics and Gynecology. 2023;229:660.el.
Refer a patient to Mayo Clinic.