Jan. 09, 2024
The Journal of Gynecologic Surgery requested that two urogynecologists at Mayo Clinic in Minnesota, Brian J. Linder, M.D., and John A. Occhino, M.D., M.S., write an invited commentary regarding minimally invasive versus open abdominal sacrocolpopexy. The commentary was published in the journal in February 2023. In this article, Dr. Linder responds to questions on this topic.
Why were you addressing abdominal prolapse repairs? Aren't many of these repairs done vaginally?
Yes. Today, more prolapse repairs nationally are done vaginally than transabdominally. However, for a variety of reasons, a significant number are done abdominally through minimally invasive — laparoscopic or robotic — or open approaches. Since the early 2000s, use of the minimally invasive approach to sacrocolpopexy has grown and now accounts for 80% or more of these surgeries.
How do you recommend a surgical approach for a patient with prolapse?
It really comes down to the patient's comorbidities and preferences. I present patients the menu of options, including various repairs, and the advantages and disadvantages. I answer their questions and let them choose which approach they want. This allows patients more involvement in decision-making, which I think is key.
Are there situations where patients commonly elect sacrocolpopexy?
One of the common scenarios is in the setting of recurrent prolapse. Here, women may choose sacrocolpopexy if a prior vaginal surgery didn't last. The second time, the patient may want abdominal surgery using mesh to do the repair differently. On the other hand, some patients prefer sacrocolpopexy as their primary operations due to its durability.
Since mesh use has been controversial, what reactions to it are you observing in patients?
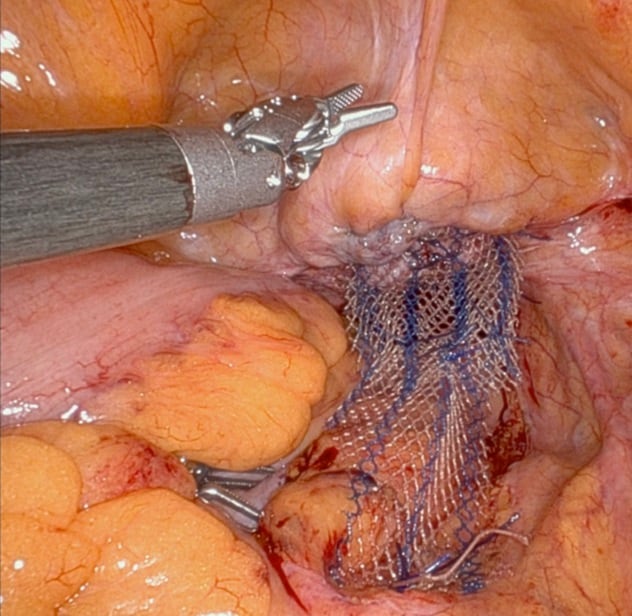 网片附件
网片附件
通过机器人阴道骶骨固定术完成的网片附件
A lot of women have questions about the use of mesh during the consult. We take the time to discuss the Food and Drug Administration statements on mesh use for prolapse, which were primarily related to transvaginal mesh placement for prolapse. This is a different application of mesh compared with a transabdominal approach with sacrocolpopexy. We explain data on mesh safety related to sacrocolpopexy, but ultimately, it's up to the patient. It's OK if a patient doesn't want surgery with mesh. The best surgical approach is what the patient feels is right; it is not one-size-fits-all.
What are the advantages and disadvantages of the minimally invasive abdominal approach?
With minimally invasive abdominal surgery, the incisions are smaller, the recovery is less painful and the rate of complications is lower, as noted in a paper we published in The Journal of Urology in 2018. The surgeon makes five 0.5-inch, side-to-side incisions, and the instruments are advanced through these incisions. With open surgery, a surgeon makes a single larger incision to get access to the abdomen. With minimally invasive sacrocolpopexy, patients leave the hospital the next day or even the same day. In comparison, patients leave the hospital in one or two days with open surgery. Also, minimally invasive sacrocolpopexy has decreased morbidity and complication risks compared with an open incision, with studies showing decreased risk of blood clots and embolism, wound infection, bleeding, and readmission, and reduced recovery time.
What is known about durability for abdominal open versus minimally invasive sacrocolpopexy?
There aren't a lot of studies currently looking at outcomes for open abdominal versus minimally invasive sacrocolpopexy. The minimally invasive technique for the surgery is anatomically based on the traditional open approach, but comparisons of long-term results are limited.
Is an open or a minimally invasive abdominal approach to sacrocolpopexy better for the surgeon?
There are ergonomic differences between the two approaches for the surgeon, but surgeon preferences likely, in part, come down to the particular surgeon's skill set. If a surgeon doesn't regularly perform robotic or laparoscopic surgery, it's likely better for that surgeon to use the open approach to sacrocolpopexy if that's what the surgeon is skilled at. This is normal for any surgery's learning curve: It takes a number of times doing a particular surgery to be efficient and minimize complications. Commonly, a higher volume of either approach means surgeons will have better outcomes with what they do most. Using the robot allows for magnification beyond what you can see on your own and angles for operating you can't access as well with open surgery.
What are the challenges for surgeons to perform an optimal sacrocolpopexy?
I'd say these are the top challenges:
- Optimizing the presacral dissection.
- Carrying the dissection far enough along the anterior and posterior vaginal walls.
- Correctly tensioning the mesh.
If you had the option of performing an open versus a minimally invasive sacrocolpopexy, which would you choose?
If I had the option of doing minimally invasive surgery using robotics, I'd do it. My surgical volumes more often involve use of the minimally invasive approach, so that's what I would lean toward. However, some of my colleagues only do open abdominal sacrocolpopexy. They have expertise in that approach and prefer the surgery that way. Their patients do well also.
Do you have any suggestions for performing an open or a minimally invasive abdominal sacrocolpopexy?
Yes. I'd suggest the following:
- Ensure adequate surgical exposure.
- Be sure to perform adequate dissections.
- Secure the mesh to reduce the prolapse but avoid over-tensioning the mesh. This is important to lower the patient's risk of developing or exacerbating stress urinary incontinence.
Does Mayo Clinic use uterine-sparing surgery for pelvic organ prolapse?
More commonly, we use uterine-sparing prolapse repairs that rely on native tissue rather than mesh-based repairs.
If I'm interested in referring patients for consults about pelvic organ prolapse, would you accept them?
Yes. We have a variety of treatment options available for prolapse and would welcome the opportunity to meet your patients and tailor treatment to their preferences.
For more information
Linder BJ, et al. Robotic-assisted surgery for pelvic organ prolapse: Sacrocolpopexy and beyond. Journal of Gynecologic Surgery. 2023;39:25.
Linder BJ, et al. A national contemporary analysis of perioperative outcomes of open versus minimally invasive sacrocolpopexy. The Journal of Urology. 2018;200:862.
Refer a patient to Mayo Clinic.