July 27, 2024
 子宫切除类型
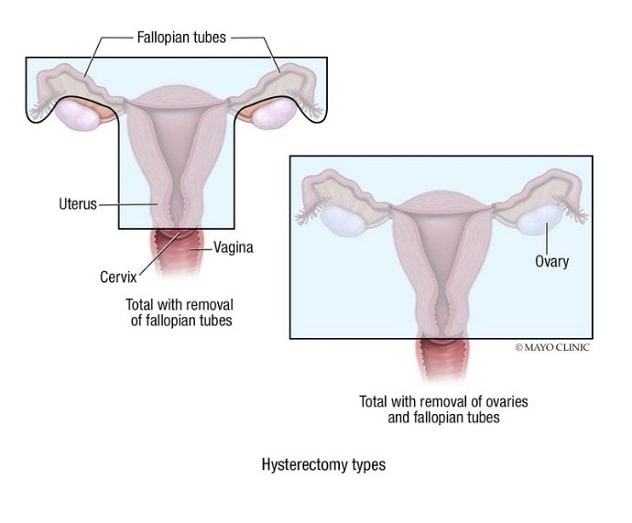
子宫切除类型
全子宫切除合并输卵管切除术和全子宫切除合并卵巢和输卵管切除术涉及的解剖学。
Findings from a multicenter study published in the Journal of Women's Health demonstrated that hysterectomy — by itself or combined with oophorectomy — and tubal ligation may increase the risk of cardiovascular disease (CVD). These findings build on previous findings linking oophorectomy and CVD as well as recent studies evaluating risks of hysterectomy alone.
Study design and findings
Using data from the Nurses' Health Study II, the investigators from Mayo Clinic, University of Arizona and other medical centers evaluated participants' medical records for CVD, including fatal coronary heart disease, fatal and nonfatal myocardial infarction, and fatal and nonfatal stroke. They also assessed patients' needs for cardiovascular revascularization, including coronary artery bypass graft surgery, angioplasty and stent placement.
"Overall, the pendulum is swinging toward being more careful with use of hysterectomy — acknowledging that there are downstream effects of this surgery," says Sarah L. Rassier, M.D., M.P.H., a Mayo Clinic gynecologist and a co-author of the Journal of Women's Health article.
According to Dr. Rassier, questions related to the uterus and ovaries that have been unanswered yet considered important in gynecologic surgery include:
- If you are in your 20s, does it make a difference to your long-term health if you have a hysterectomy? What about in your upper 40s?
- Are women prone to having a hysterectomy inherently different than other women? Are there predisposing factors?
- Does the uterus have a yet-to-be-determined purpose other than just structure/ and fertility?
- By taking away the uterus, does the blood supply to the ovaries diminish?
To solve the first of these questions, the investigators evaluated Nurses' Health Study II participant data from 1989 to 2017. At the start of the Nurses' Health Study II, the average participant's age was 34. Over the course of the study, 1,864 patients had CVD. The greatest CVD risk arose in women who underwent hysterectomy with bilateral (HR 1.27) or unilateral oophorectomy (HR 1.4). The investigators noted increased risk of CVD plus coronary revascularization in women who only had hysterectomy (HR 1.19), hysterectomy plus unilateral oophorectomy (HR 1.29), hysterectomy plus bilateral oophorectomy (HR 1.22) and tubal ligation (HR 1.16).
The investigators found that age at the time of the surgical procedures impacted the risk of CVD and cardiac revascularization, with women who had surgery prior to age 50 exhibiting greater risk.
They also noted that hysterectomy — regardless of whether the patient keeps the ovaries — does affect CVD risk.
One downside to this study is that participants represent a fairly homogenous female group who are medically literate and have higher socioeconomic status, says Dr. Rassier.
"It doesn't mean you shouldn't have a hysterectomy, but you have to look at the risk-benefit ratio for you as an individual."
Applications of these findings for patient care
Decisions about hysterectomy, oophorectomy and tubal ligation often are not clear-cut, says Dr. Rassier. She says it is one thing for a physician to be familiar with epidemiological studies on these surgeries, but it is another thing to have a patient sitting in front of you needing to decide whether to proceed. She says the decision whether to pursue these surgeries is complex and that the patient and physician should discuss all options thoroughly.
Dr. Rassier indicates that gynecologists use hysterectomy to treat many conditions and that its use should be carefully considered going forward.
"It doesn't mean you shouldn't have a hysterectomy, but you have to look at the risk-benefit ratio for you as an individual," she says.
An example of the individualization Dr. Rassier proposes for decisions about pursuing hysterectomy to treat a given condition might involve consideration of whether a patient has a family history of CVD. If so, the surgeon and the patient must consider this factor before undertaking a hysterectomy.
"It's not that you can't have a hysterectomy," she says. "The message is that hysterectomy should not be a knee-jerk intervention, but rather considered as one option among others."
Dr. Rassier says some patients may have significant reasons that might outweigh the risks of going forward with a hysterectomy.
Though the patient and physician should discuss the patient's risks and benefits related to a tubal ligation, hysterectomy, or a hysterectomy plus unilateral or bilateral oophorectomy, Dr. Rassier notes that no algorithm exists to expedite this decision.
"This study gives us more information, but you can't just plug a patient into an equation to understand their risk," she says.
The patient group Dr. Rassier predicts these findings will affect most is those with abnormal bleeding who are uninterested in medical therapy and only want to pursue hysterectomy. She suggests that these patients and their gynecologists should deeply consider hysterectomy alternatives.
"There is a reason for all OB-GYNs to be aware of and follow the data on these gynecologic surgeries: So they can offer the best information to their patients," she says.
If your patient would like to have a gynecologic surgery that is not your top recommendation, that individual should have the right to decide, says Dr. Rassier.
"We are not the gatekeepers," she says. "Ultimately — providing the surgery isn't something medically inappropriate — the patient does not have to go with our recommendations."
Future studies
In the future, Dr. Rassier hopes a study similar to the Nurses' Health Study II will include more nonwhite women; additional information on the reasons women decide to proceed with a hysterectomy, oophorectomy or both; and more-detailed information about participant hormone therapy, if applicable. She also would like to see an evaluation of the CVD effects of hysterectomy, oophorectomy and tubal ligation in younger women.
For more information
Farland LV, et al. Hysterectomy with and without oophorectomy, tubal ligation, and risk of cardiovascular disease in the Nurses' Health Study II. Journal of Women's Health. 2023;32:747.
Refer a patient to Mayo Clinic.