March 18, 2025
Obstetricians must identify early all patients with hypertensive disorders of pregnancy (HDP) — a group of diseases including chronic hypertension, gestational hypertension, preeclampsia, eclampsia and HELLP syndrome — according to an editorial in JAMA Network Open by three obstetrics and nephrology and hypertension investigators from Mayo Clinic's campus in Minnesota. Although there is currently no cure for HDP, physicians can surveil patients through regular blood pressure (BP) measurements throughout pregnancy and enable delivery at the appropriate gestational age to prevent complications for the patient and infant, according to a 2020 publication in Obstetrics & Gynecology.
HDP is on the rise, mostly due to increased obesity and maternal age, which leads to higher comorbidity rates, says Janelle Santos, M.D., a maternal-fetal medicine specialist at Mayo Clinic in Minnesota. In 2019, hospitals reported that 15.9% of delivering patients had HDP, while the rate was 13.3% in 2017, according to Ford and colleagues in a 2022 publication in Morbidity and Mortality Weekly Report. HDP also affects populations disproportionately with non-Hispanic Black, American Indian and Alaska Native people having higher risk compared with their white counterparts. Pregnant patients in the lowest 25% of U.S. income or who deliver infants in the Midwest or South are also at increased risk.
"We know that there's a connection with lower socioeconomics and HDP, related to lack of preventive healthcare and diet," says Dr. Santos.
Preeclampsia is one of the more severe forms of HDP for which the only cure is delivery. If preeclampsia occurs late in the patient's pregnancy, physicians may proceed to deliver the infant. However, if preeclampsia arises earlier in the pregnancy, complications of prematurity become a concern. In these cases, Dr. Santos says physicians carefully balance maternal health with fetal health to come to the best management strategy. She says that typically, preeclampsia worsens throughout pregnancy.
"We don't see preeclampsia getting better as the pregnancy progresses," she says.
If the plan is to continue the pregnancy, obstetricians may prescribe antihypertensives or admit for more intensive monitoring until delivery. They also can use magnesium to prevent complications from preeclampsia. Preeclampsia also may increase the likelihood of needing a C-section.
National and JAMA Network Open author recommendations
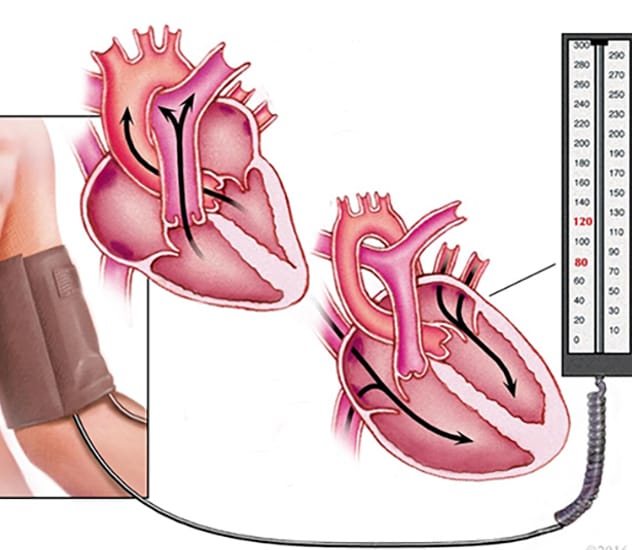 血压测量
血压测量
测量舒张压和收缩压,以监测高血压。
In 2017, the U.S. Preventive Services Task Force (USPSTF) recommended measuring patients' blood pressure throughout pregnancy for preeclampsia detection. In 2023, this same body updated the recommendation to screening for HDP due to the ease of blood pressure monitoring and the potential morbidity of HDP for patients and infants, according to the USPSTF's publication in JAMA. This task force also considered results for multiple screening mechanisms.
"Tight blood pressure control prevents preeclampsia, especially with the use of antihypertensives and aspirin," says Dr. Santos.
The Mayo Clinic authors of the JAMA Network Open editorial also recommended the following:
- Home blood pressure monitoring is unnecessary. A 2022 study of home blood pressure monitoring by Tucker and colleagues, published in JAMA, did not lead to a higher rate of HDP diagnoses. Given the time span needed to determine the presence of HDP, preeclampsia diagnosis rates or perinatal outcomes, home BP monitoring was deemed unnecessary.
- Fewer prenatal checkups for patients at low risk. If patients were determined to be low risk, having reduced prenatal visits did not alter perinatal outcomes. The USPSTF determined this from a review of a study by McDuffie and colleagues published in JAMA in 1996, in addition to two other studies.
- No across-the-board screening for proteinuria. A nonrandomized study by Rhode and colleagues, published in the Journal of Reproductive Medicine, indicated urine screening did not produce higher HDP diagnosis compared with regular BP measurement.
Other recommendations of the editorial authors
The Mayo Clinic authors also make recommendations for the care of patients previously diagnosed with hypertension or who may develop HDP:
- Hypertension is serious, and medical professionals should prioritize its treatment. This is critical so that the obstetrician can keep a close eye on any patient who is pregnant and has had or develops hypertension, noting that hypertension can worsen quickly.
- Precautions for hopeful parents with chronic hypertension. Dr. Santos recommends that a patient who intends to become pregnant and has a diagnosis of chronic hypertension meet with a maternal-fetal medicine specialist, if available, or an obstetrician familiar with chronic hypertension. She believes it is important to manage conditions related to chronic hypertension prior to conception.
- Addressing the socioeconomic factors increasing HDP rates in select populations. The authors believe that these factors must be addressed in a multifaceted manner, including increased outreach and diversity in obstetrics staff.
- Seek consult or refer patients with chronic hypertension or HDP to a maternal-fetal medicine specialist. At Mayo Clinic in Minnesota, for example, maternal-fetal medicine specialists consult with external physicians by phone regarding how to manage patients' hypertension locally or suggest a referral if needed. She says that Mayo Clinic always has a maternal-fetal medicine specialist on call who is responsible for inquiries from other medical professionals by phone, email or Epic chat.
For more information
Santos J, et al. Early identification of individuals at risk for hypertensive disorders of pregnancy. JAMA Network Open. 2023;6:e2334858.
American College of Obstetricians and Gynecologists. Practice Bulletin No. 222: Gestational hypertension and preeclampsia. Obstetrics & Gynecology. 2020;135:1492.
Ford ND, et al. Hypertensive disorders in pregnancy and mortality at delivery hospitalization — United States, 2017-2019. Morbidity and Mortality Weekly Report (MMWR). 2022; 71:585.
U.S. Preventive Services Task Force. Screening for hypertensive disorders of pregnancy. JAMA. 2023;330:1074.
Rhode MA, et al. Indicated vs. routine prenatal urine chemical reagent strip testing. Journal of Reproductive Medicine. 2007;52:214.
Tucker KL, et al. Effect of self-monitoring of blood pressure on diagnosis of hypertension during higher-risk pregnancy: The BUMP 1 randomized clinical trial. JAMA. 2022;327:1656.
McDuffie RS Jr, et al. Effect of frequency of prenatal care visits on perinatal outcome among low-risk women: A randomized controlled trial. JAMA. 1996;275:847.
Refer a patient to Mayo Clinic.