Jan. 28, 2025
Diagnosing moyamoya disease is challenging, as the disease has many mimics. Treatment decisions also are complicated by the complex hemodynamics of this rare condition. Mayo Clinic's moyamoya imaging protocol is aimed at a comprehensive assessment of underlying hemodynamic and physiological alterations to better guide patient care.
"A structural overview of blood vessels is important, but it isn't the whole story. Our protocol also involves a more comprehensive assessment of the severity of hemodynamic effects for each individual patient," says Girish Bathla, M.B.B.S., M.MED, a neuroradiologist at Mayo Clinic in Rochester, Minnesota.
Moyamoya disease is a progressive condition characterized by blockage in the distal internal carotid artery and adjacent blood vessels. The name moyamoya, which means "puff of smoke" in Japanese, describes the appearance of the tangle of tiny blood vessels formed to compensate for the blockage. Moyamoya disease can have devastating consequences, including stroke and seizure in children and young adults.
Mayo Clinic's imaging protocol, developed in-house, combines several MRI components. When feasible, 7T MRI is used for enhanced clarity. Testing is performed in a single session and includes:
- MRI to identify infarcts and white matter changes.
- Vessel wall imaging to evaluate vessel wall thickening and enhancement.
- 3D time-of-flight magnetic resonance angiography (3D-TOF MRA) to evaluate areas of vascular stenosis.
- Blood oxygenation level-dependent (BOLD) functional MRI to assess cerebrovascular reserve.
- Dynamic susceptibility contrast perfusion imaging to evaluate hemodynamic effects of underlying vasculopathy.
"We have the most updated scanners and sequences and a very cohesive working environment with Neurologic Surgery and Neurology," Dr. Bathla says. "That allows us to envision the best way forward for each patient."
Highly detailed imaging
Moyamoya disease can occur at any age, but symptoms are most common in children ages 5 to 10 and adults ages 30 to 50. As a referral center, Mayo Clinic has extensive experience with managing the disease. Neuroradiologists, neurologists and neurosurgeons at all three of Mayo Clinic's campuses work as a team to determine optimal treatment.
"We want to diagnose moyamoya disease early and select patients who are at risk of future strokes and require surgery — versus patients who can be managed with medical therapy alone," says Giuseppe Lanzino, M.D., a cerebrovascular neurosurgeon at Mayo Clinic's campus in Minnesota.
Individuals with moyamoya disease require lifelong care. Mayo Clinic performs regular follow-up imaging and clinical visits to determine whether surgery has been successful and to monitor patients who have been treated with medical therapy alone. The same imaging protocol is used at each visit. "That consistency is important for determining serial changes," Dr. Bathla says.
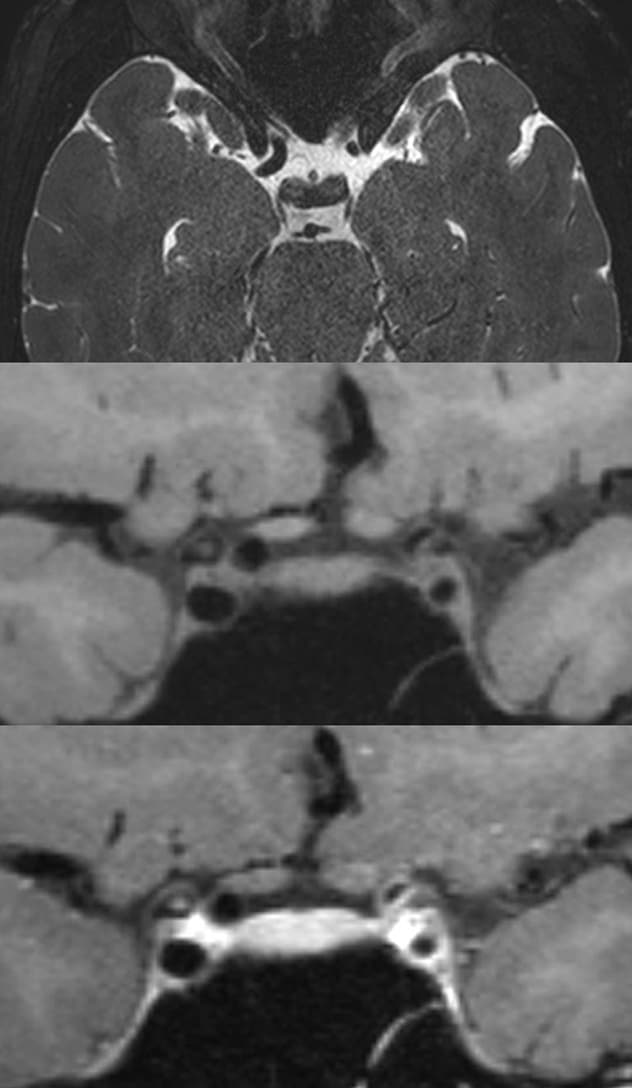 T2-weighted MRI
T2-weighted MRI
Vessel wall imaging of a patient with moyamoya disease. Axial T2 image shows narrowed internal carotid artery on the left side with negative remodeling (top). Associated wall thickening (middle) and enhancement (bottom) are visible.
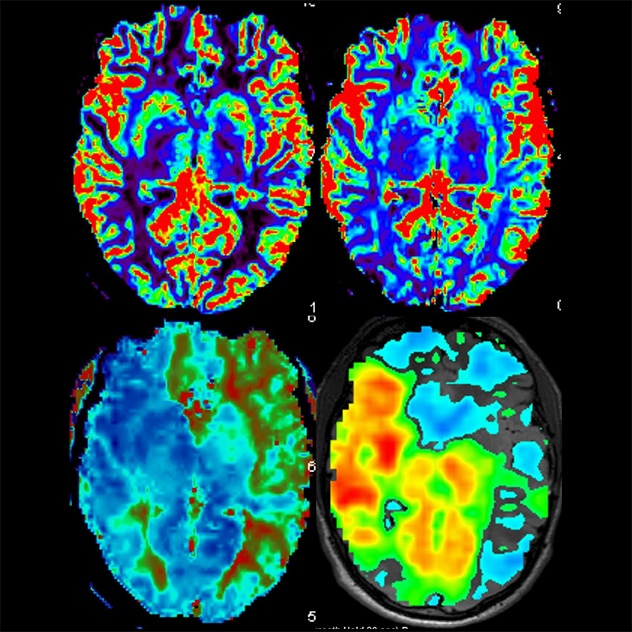 MRI perfusion imaging
MRI perfusion imaging
MR perfusion and breath-hold images of a patient with moyamoya disease reveal preserved relative blood flow (top left), mildly elevated relative blood volume (top right), increased thrombotic thrombocytopenic purpura (bottom left) and reduced cerebrovascular reserve (bottom right), predominantly along the left middle cerebral artery and bilateral anterior cerebral artery distributions.
Testing starts with high-resolution MRI to identify infarcts. "For follow-up monitoring, we want to see if there are any white matter changes or telltale signs of reduced blood flow since the prior study," Dr. Bathla says.
MRI of the cerebral vessel walls is then performed. "We use a fairly high resolution — around 0.5- to 0.55-mm isotropic voxel on 3T MRI machines and about 0.3-mm isotropic voxel size on 7T," Dr. Bathla says. "We use not just T1-weighted images but also T2-weighted images."
T1-weighted imaging measures vessel wall thickness and can visualize wall enhancement postcontrast. T2-weighted imaging — which better evaluates wall remodeling — can help visualize lenticulostriate collaterals and differentiate moyamoya disease from atherosclerotic disease. Imaging also helps determine extent of involvement and the presence of unilateral or bilateral lesions, as well as involvement of posterior circulation.
3D-TOF MRA is performed to evaluate larger intracranial arterial vessels, moyamoya collaterals and direct bypass grafts. "This test gives us a good idea of areas of slow blood flow or focal stenosis," Dr. Bathla says.
BOLD functional MRI is used to assess any reductions in cerebrovascular reserve. "Individuals with impaired cerebrovascular reserve are 'maxed-out' in terms of vasodilation and may be symptomatic or have higher risk of stroke when under physiological stress," Dr. Bathla says. "We perform breath-hold imaging to determine which areas of brain tissue aren't able to compensate for hypoxia."
Finally, perfusion imaging helps further assess the underlying hemodynamic derangements in semiquantitative parameters by assessing the relative blood flow, blood volume and time-dependent variables.
State-of-the-art imaging is at the heart of Mayo Clinic's approach to patient care. "We have a problem-solving attitude. All our specialists want to work together to solve whatever problems patients might have," Dr. Bathla says.
For more information
Refer a patient to Mayo Clinic.