Oct. 27, 2023
Mayo Clinic stresses multidisciplinary management of pituitary tumors, to optimize surgical outcomes. A subspecialized team of neurosurgeons, endocrinologists, ENT/head and neck surgeons, and radiation oncologists work together to provide patient-centered care.
"We have a high-volume practice in pituitary tumors and a very high cure rate. The neurosurgeons who manage these patients have fellowship training in pituitary surgery," says Kaisorn L. Chaichana, M.D., a neurosurgeon at Mayo Clinic in Jacksonville, Florida.
Precise imaging and surgical expertise are needed to pinpoint tumor location, maximize resection and avoid morbidity. "That can be achieved with experienced hands at an experienced center," Dr. Chaichana says. "Our goal is to return our patients to normal quality of life."
Subspecialized expertise
Pituitary adenomas comprise 10% to 15% of all intracranial tumors. At Mayo Clinic, patient care generally starts in endocrinology. Comprehensive clinical assessment includes evaluation of comorbidities associated with functional tumors or hypopituitarism, including dynamic pituitary testing and inferior petrosal sinus sampling.
Mayo Clinic's 7T MRI can be used to identify pituitary tumors. Scanning at 7T is made challenging by a characteristic artifact from the skull base, which can obscure the pituitary gland. But Mayo Clinic's MRI physicists have discovered ways to mitigate that artifact.
"Our goal is to return our patients to normal quality of life."
The multidisciplinary pituitary tumor team meets to discuss each individual's test results and recommend treatment. Tumors producing prolactin are generally treated with medical therapy. Tumors producing cortisol or growth hormone are candidates for surgical resection. Nonfunctioning tumors also are surgically resected if they are growing or pressing on the optic nerve.
 肢端肥大症治疗
肢端肥大症治疗
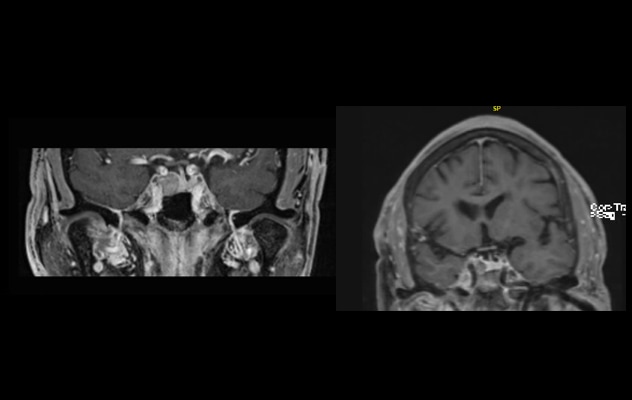
左侧 MRI 显示的腺瘤导致肢端肥大症伴生长激素升高。这名 56 岁患者的症状包括关节疼痛、高血压以及面部和手部改变。右侧为内镜经鼻蝶手术后的 MRI 图像,显示已切除腺瘤。患者于术后第二天出院回家,使用激素治疗,3 年后仍处于缓解期。
Endoscopic transnasal transsphenoidal surgery is generally performed. "It's the least invasive approach," Dr. Chaichana says. "It also maximizes visualization because it allows us to go right up to the surgical field." Mayo Clinic was among the first centers to extensively research this technique.
A neurosurgeon and an ENT/head and neck surgeon collaborate on each procedure. "No incisions are made. We use the natural corridors — the sinuses in the skull — to access the pituitary gland," Dr. Chaichana says.
Doppler ultrasound is used to help identify and avoid arteries. About 95% of patients return home the day after pituitary tumor surgery.
"Pituitary tumors vary greatly. This is a heterogenous group of patients," Dr. Chaichana says. "But pituitary surgery is generally safe and effective, when performed at a center with experience and expertise."
For more information
Refer a patient to Mayo Clinic.