June 20, 2024
Mayo Clinic offers the world's first multidisciplinary clinic devoted to myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD). The MOGAD Clinic's subspecialized team can provide quick and accurate diagnosis and a care plan for this newly defined autoimmune disorder.
"This is a rare demyelinating condition. Early diagnosis is important because there's evidence that treating within seven days of symptom onset reduces the likelihood of residual deficits," says Eoin P. Flanagan, M.B., B.Ch., a Mayo Clinic autoimmune neurologist.
Mayo Clinic's autoimmune neurologists have been at the forefront of efforts to define MOGAD as a clinical entity and to find treatments. The disease can be mistakenly diagnosed as multiple sclerosis (MS) or aquaporin-4-IgG-positive neuromyelitis optica spectrum disorder (AQP4+NMOSD). But those diseases have different long-term sequelae and require different treatment approaches.
 病变的发展
病变的发展
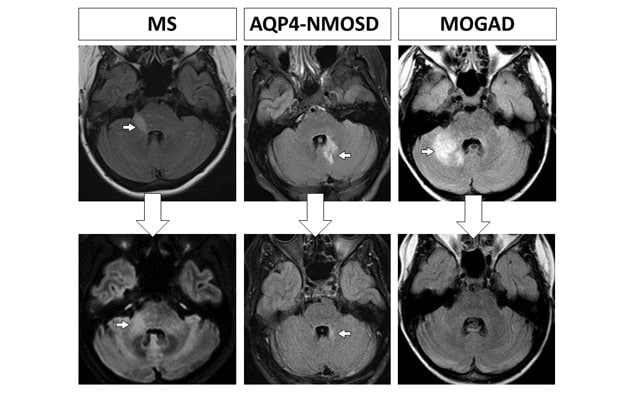
在上面一行,脑部 MRI 扫描显示多发性硬化症(MS)、水通道蛋白 4 IgG 阳性的视神经脊髓炎谱系疾病(AQP4-IgG-NMOSD)和髓鞘少突胶质细胞糖蛋白抗体相关疾病(MOGAD)发作时出现的病变(如箭头所示)。在下面一行,几个月至几年后进行的随访 MRI 显示 MS 病变留下的中等大小的疤痕(如箭头所示)和 AQP4+NMOSD 病变留下的小疤痕(如箭头所示)。随访 MOGAD 扫描显示病变完全消退。
"T2-weighted MRI has shown that lesions completely resolve more frequently with MOGAD than with MS or AQP4+NMOSD," Dr. Flanagan says. "Also, because about half of patients with MOGAD have monophasic disease, attack-prevention treatment is usually recommended only after a second clinical event."
Mayo Clinic has evaluated hundreds of pediatric and adult patients for MOGAD. The MOGAD Clinic care team includes specialists in:
- Neurology.
- Neuroimmunology.
- Neuro-ophthalmology.
- Physical medicine and rehabilitation.
- Urology.
- Neuropsychology.
- Neuroradiology.
- Pediatric neurology
- Pain medicine.
- Laboratory medicine and pathology.
"A multidisciplinary clinic can be beneficial to determining the exact diagnosis," Dr. Flanagan says. "We also have experience in recommending the optimal treatment approach."
Diagnostic expertise
Although rare, MOGAD affects more than 300,000 people worldwide and up to 17,000 people in the United States alone. Mayo Clinic neurologists were part of the international group that established the diagnostic criteria for the condition in 2023.
MOGAD symptoms include:
- Vision loss.
- Muscle weakness, stiffness or paralysis.
- Unsteady gait.
- Sensory loss and changes in bowel, bladder or sexual function.
- Cognitive impairment.
- Seizures.
- Headache.
"These symptoms arise from optic neuritis, transverse myelitis and acute disseminated encephalomyelitis, which can also occur with other conditions. This is why MOGAD can be misdiagnosed," Dr. Flanagan says.
Diagnosis requires a serum test positive for the presence of myelin oligodendrocyte glycoprotein (MOG) antibodies. As described in JAMA Neurology, Mayo Clinic researchers confirmed MOG antibodies as a biomarker for MOGAD. Mayo Clinic also was the first center in the United States to develop a MOG antibody test and is the only center to use the live cell-based assay that is considered the gold standard and is available through Mayo Clinic Laboratories.
"Having a laboratory on site allows us to analyze the antibody test in detail," Dr. Flanagan says.
Mayo Clinic is now developing a cerebrospinal fluid test for MOG antibodies. This type of test appears to have utility, as explained in Annals of Neurology.
"A level of clinical experience and focus on MOGAD is important to determining if patients truly have the disease."
Dr. Flanagan notes that low levels of MOG antibodies can occur in 1% to 2% of other diseases. "Caution is needed in terms of potential false positives," he says. "A level of clinical experience and focus on MOGAD is important to determining if patients truly have the disease."
MRI expertise also is needed. "MOGAD has some particular imaging characteristics that are important for neuroradiologists to recognize," says P. Pearse P. Morris, M.B., B.Ch., a neuroradiologist at Mayo Clinic's campus in Minnesota. "There are substantial ramifications from confusing MOGAD with MS or NMOSD. The treatments and patient counselling on prognosis are quite different."
In a study published in Neurology, Mayo Clinic researchers showed that most T2-MRI lesions in MOGAD resolve — unlike MS, in which almost all lesions persist and form scars. Key MRI findings for NMOSD and MOGAD were elucidated in a review published in Neurologic Clinics.
"Recognizing these MRI features helps select those patients who should be tested for MOG and AQP4 antibodies," Dr. Flanagan says.
Treatment options
MOGAD attacks are often severe. "Recovering from these attacks can take weeks or months, and disability usually gets worse after each attack," Dr. Flanagan says.
Treatment options include high-dose corticosteroids, plasma exchange or, less commonly, intravenous immunoglobulin (IVIG). Immunosuppressants might be recommended for people who experience severe, recurrent attacks.
"Adults with early relapses should be considered for long-term immunosuppressants, particularly if they have multiple early attacks," Dr. Flanagan says. "Long-term studies are needed to assess if there is a safe or optimal time to stop immunosuppressants in relapsing patients."
Mayo Clinic researchers are participating in clinical trials of new treatments that can prevent MOGAD attacks. "We are also conducting observational research studies that assess the MOG antibody titers over time and that look at various aspects of MOGAD, so we can better understand and treat the disease," Dr. Flanagan says.
Early, aggressive treatment can help people with severe symptoms regain function. "That shows the power of the field of autoimmune neurology," Dr. Flanagan says. "As a center of expertise, the MOGAD Clinic can really help people get back to the best of their lives."
For more information
MOGAD Clinic. Mayo Clinic.
Mayo Clinic Laboratories.
Sechi E, et al. Positive predictive value of myelin oligodendrocyte glycoprotein autoantibody testing. JAMA Neurology. 2021;78:741.
Redenbaugh V, et al. Diagnostic utility of MOG antibody testing in cerebrospinal fluid. Annals of Neurology. In press.
Sechi E, et al. Comparison of MRI lesion evolution in different central nervous system demyelinating disorders. Neurology. 2021;97:e1097.
Cacciaguerra L, et al. Updates in NMOSD and MOGAD diagnosis and treatment. Neurologic Clinics. 2024;42:77.
Refer a patient to Mayo Clinic.