June 20, 2024
Mayo Clinic is committed to using the best technology to manage epilepsy. Magnetoencephalography (MEG) — a noninvasive test to help identify seizure-origin locations for patients with focal epilepsy — is now available.
"This tool will help us target locations for stereo-electroencephalography (sEEG) electrode placement, to verify possible sites of seizure onset before epilepsy surgery," says Jeffrey W. Britton, M.D., a Mayo Clinic neurologist. "The goal is to enhance the precision and improve outcomes for these patients."
Mayo Clinic will be one of a few centers in the United States to routinely offer MEG. The technology records, analyzes and localizes minute magnetic fields produced by the brain's electrical currents. With the help of mathematical modeling, abnormal magnetic fields are then superimposed onto an MRI scan of the patient's brain to pinpoint the source of abnormal activity.
"This technology allows us to better look at abnormal discharges in the brain that occur in patients with seizures, which is an important biomarker for a potential seizure focus," says Jamie J. Van Gompel, M.D., a Mayo Clinic neurosurgeon. "We cannot see most of the seizure onset zones on imaging. Techniques like MEG are super helpful in allowing us potentially to find the seizure-starting spot, test it — and then treat it."
 放置引导电极
放置引导电极
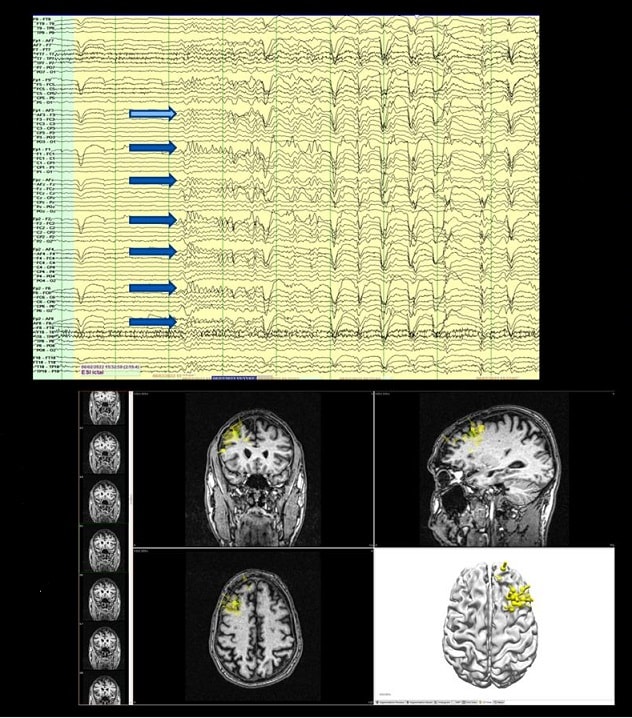
一位局灶性癫痫患者的脑电图显示多个可能的癫痫发作起源的脑区(蓝色箭头)。患者没有植入一系列电极来定位癫痫发作的起源位置,而是进行了脑磁图检查。黄色点簇表明可能的癫痫发作起源位置,从而减少了植入的电极数量。
MEG analyzes magnetic signals created by abnormal discharges from neurons firing in synchronous bursts. In areas where seizures organize, groups of brain cells fire in step with one another, producing small currents that give rise to small magnetic fields. MEG provides views of the magnetic fields produced by this activity, which helps locate the area of seizure origin.
MEG is suitable for patients of all ages. The procedure takes about two hours. The patient's head is placed in a helmet lined with hundreds of magnetic sensors. The patient lies still or completes a series of tasks, such as listening to words or looking at pictures. An EEG is recorded at the same time to help correlate the findings.
"Sedation services will be available for small children or adults when needed," Dr. Britton says.
The MEG recording collects normal and abnormal brain signals during every millisecond of the study. "Analyzing the studies takes a lot of effort and expertise," Dr. Britton says. "The raw data are marked, and from there a computer generates the possible sources of abnormal activity. There are many opportunities for artificial intelligence and machine learning to help us refine and improve the efficiency of this analysis."
"Techniques like MEG are super helpful in allowing us potentially to find the seizure-starting spot, test it — and then treat it."
Neurostimulation options for epilepsy
When surgical resection isn't feasible, neurostimulation might be used to treat epilepsy. That approach is often used in addition to medication, to reduce the number of seizures and lower their intensity.
Mayo Clinic specialists have extensive experience with:
- Vagus nerve stimulation (VNS), which uses a device implanted under the skin in the chest to send regular, mild pulses of electrical energy to the vagus nerve, leading indirectly to improvements in brain excitability.
- Responsive neurostimulation (RNS), which involves a cranial device that targets the seizure focus and monitors brain waves to detect the onset of seizures and stop them before they progress.
- Deep brain stimulation (DBS), which delivers controlled pulses to the thalamus to interrupt circuits involved in seizures.
- Chronic subthreshold stimulation, which provides continuous electrical impulses to an area of seizure onset to suppress the generation of the abnormal seizure-related discharges.
- Transcranial magnetic stimulation (TMS), which uses an electromagnetic coil placed against the scalp to stimulate neurons in the brain and guide mapping and treatment.
- Transcranial direct current stimulation (tCDCS), which passes a weak electrical current between sponges placed on the scalp, leading to reduced brain excitability.
Except for transcranial neurostimulation methods, these therapies require surgical implantation.
"While the thought of undergoing implantation of a device can be scary to think about, the complication rate of these implantation procedures is very low in the hands of our exceptional neurosurgery colleagues," Dr. Britton says. "Neurostimulation doesn't bring quick results. But many people who have used these treatments notice a positive difference over time."
For more information
Refer a patient to Mayo Clinic.