Oct. 26, 2024
As a high-volume center, Mayo Clinic has deep experience treating people with the diverse range of benign brain neoplasms. That expertise facilitates comprehensive care at diagnosis as well as primary, salvage and revision surgeries.
"We are one of the highest volume benign tumor practices in the country, by far," says Jamie J. Van Gompel, M.D., a neurosurgeon at Mayo Clinic's campus in Minnesota. "When you see a lot of everything, you can start to notice the differences in outcomes from using various techniques — the little things that matter. That makes you think outside the box about how you truly can help patients."
A multidisciplinary approach is key to optimizing outcomes. "We've built a large group of neurosurgeons, ENT/head and neck surgeons, and radiologists who routinely work together. None of us has a financial incentive not to work as a team," says Michael J. Link, M.D., a neurosurgeon at Mayo Clinic's campus in Minnesota. Depending on the tumor type, the treatment team also might include endocrinologists, neuro-ophthalmologists, neuro-oncologists, radiation oncologists, audiologists and psychologists.
Advanced technology is used to guide treatment plans. "These tumors are located in very delicate areas. Using the latest MRI and other technologies allows us to understand the relationship between the tumor, brain and other important structures," says Maria Peris Celda, M.D., Ph.D., a neurosurgeon at Mayo Clinic's campus in Minnesota. "Our subspecialized treatment team routinely manages complex tumors."
State-of-the-art imaging
 肿瘤识别
肿瘤识别
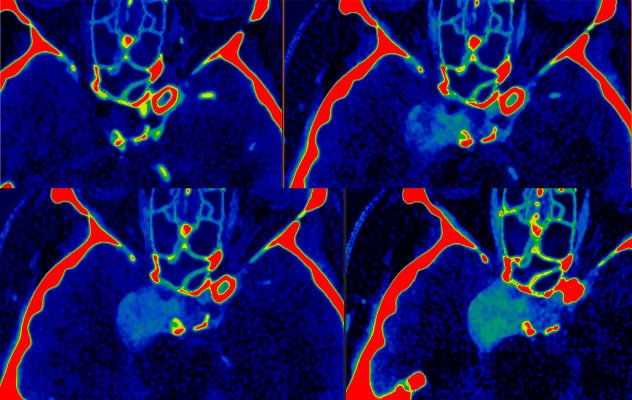
光子计数探测器 CT 成像碘图显示肿瘤逐渐充满,这是血管瘤的特征。多相显像有助于精确诊断。
Comprehensive care starts with precise initial diagnosis. Mayo Clinic uses state-of-the-art imaging to evaluate benign neoplasms and plan surgical approaches. DOTATATE-PET, a new technology, provides accurate mapping for meningioma resections. Photon-counting detector CT is a technology developed at Mayo Clinic that offers enhanced spatial resolution.
"Compared with conventional CT, photon-counting detector CT gives us thinner slices and brighter contrast," says Ian T. Mark, M.D., MSM, a neuroradiologist at Mayo Clinic's campus in Minnesota. Temporal resolution also is enhanced, allowing for faster scanning time.
Contrast-enhanced MRI sequences include double inversion recovery, fast imaging employing steady-state acquisition-constructive interference in steady state (FIESTA-CISS) and submillimeter 3D dynamic pulse Cartesian acquisition with projection reconstruction-like (pCAPR) sampling. "Traditional dynamic MRI imaging of the pituitary results in 2D slices that are relatively thick — about 2 to 3 mm," Dr. Mark says. "But our new pCAPR technique gives us 3D submillimeter slices."
Managing complex conditions
Mayo Clinic surgeons frequently perform revision surgeries for individuals whose tumors have recurred or who had suboptimal outcomes at other centers.
"Because we see so many patients, we have experience with niche and nuanced conditions," Dr. Van Gompel says. "For example, we are getting more referrals for completion resections of sagittal sinus meningiomas. Those tumors typically are resected up to the sinus, leaving small amounts of tumor. But if the molecular features are that of an aggressive tumor, then removing the additional tumor may be of benefit to the patient. That has become a niche procedure."
"We are one of the highest volume benign tumor practices in the country, by far."
Molecular diagnosis is an increasingly important aspect of planning treatment. "Cytogenetic transfers and other molecular markers are part of that context that matters when seeing patients with complex problems, especially chordomas," Dr. Van Gompel says.
Augmented technologies also play a growing role. Cochlear implants are an option to preserve hearing for some individuals with small vestibular schwannomas. "Resecting these tumors can damage the nerve, and radiation can cause hearing loss. But if we can preserve the nerve, then a cochlear implant often restores some hearing," Dr. Link says.
As described in Otology & Neurotology, Mayo Clinic specialists sometimes can perform radiosurgery and implant cochlear implants in a single day. "It's a convenience for patients who have to travel to us," Dr. Link says.
Preserving quality of life is a key concern. Special attention is paid to preserving or correcting facial nerve function after tumor resection. "Facial paralysis is obviously a cosmetic problem. But it’s also a functional problem because it can slur speech, make chewing difficult and cause dry eye due to the inability to blink," Dr. Link says.
Data-based predictions
Choosing optimal strategies for managing benign neoplasms is challenging, due to the tumors' varied behavior and potential treatment complications. Mayo Clinic analyzes in-house data to facilitate patient counseling and decision-making, Factors such as patients' ages and tumor characteristics are considered.
"That allows us to come up with a prediction, based on our experience, of patients' risks for things like facial weakness or incomplete tumor resection," Dr. Link says. "Patients have more information up front."
Mayo Clinic's extensive benign neoplasm practice enables that level of care. "We are resource-rich, and the needs of the patient always come first," Dr. Van Gompel says.
For more information
Macielak RJ, et al. Coordinated same- or next-day radiosurgery and cochlear implantation for vestibular schwannoma. Otology & Neurotology. 2024;45:430.
Refer a patient to Mayo Clinic.