Aug. 30, 2024
Gliomas inevitably recur, typically within the prior treatment field and often more aggressively than the original tumor. Mayo Clinic clinician-researchers are exploring ways to prevent that recurrence and improve patients' survival.
Some of these efforts involve window of opportunity trials in which select patients are given experimental medications before tumor surgery. This allows researchers to analyze the resected tumor, determine whether the medication reached it and, if so, find out what effect it had.
"More often than not, multi-million-dollar trials have been done with drugs that didn't cross the blood-brain barrier, or at least not in sufficient concentrations to be beneficial. Window of opportunity trials are designed to give us a better sense of a drug's likely success before we start a big clinical trial," says Ian F. Parney, M.D., Ph.D., a neurosurgeon at Mayo Clinic in Rochester, Minnesota.
Other work involves ways to quickly assess treatment results and to structure clinical trials so that patients have access to the best available therapies. "Ongoing efforts could fundamentally transform our approach to clinical trials and patient care," says Mayo Clinic neurosurgeon Terry C. Burns, M.D., Ph.D., who leads the Mayo Clinic Comprehensive Cancer Center's neuro-oncology disease group.
Progress in treating brain tumors has lagged compared with that in other types of cancer. Individuals with glioblastoma — the most common glioma — survive on average 16 months after diagnosis. As a major center for brain tumors, Mayo Clinic is on the leading edge of finding new treatment approaches.
"The neuro-oncology community's lack of success in moving the needle for patients is driving us to do things differently," Dr. Parney says. "There's a desperate need to do better."
Crossing the blood-brain barrier
Clinical trials of glioma therapeutics often involve medications used to treat other types of tumors. But brain tumors' unique biology, and the challenges of crossing the blood-brain barrier, can limit those drugs' ability to treat glioma.
"Being a little more thoughtful before drugs are used in big trials can help us understand what we might do to improve a drug's effectiveness against glioma, or whether we should move on to a different drug," Dr. Parney says. "Many drugs are potentially eligible for window of opportunity trials."
One ongoing trial evaluates a combination of two immune therapies: pembrolizumab, which is an immune checkpoint inhibitor, and NT-I7, a stabilized version of interleukin-7. Patients with recurrent glioblastoma receive the medications before resection.
"Our study is ongoing, but we are seeing impacts — within tumor tissue and cerebrospinal fluid and systemically — that we wouldn't know about if the trial were not designed as a window of opportunity study," Dr. Parney says.
Another study focuses on newly diagnosed glioblastoma. Before surgery, patients take a medication that targets the MDM2-p53 pathway that regulates apoptosis and senescence. The work is being performed in conjunction with the Glioblastoma Therapeutics Network, a National Cancer Institute program to develop and test novel therapies. Dr. Parney co-directs the network coordination center, which harmonizes the group's scientific and clinical activities.
"The neuro-oncology community's lack of success in moving the needle for patients is driving us to do things differently."
He and his colleagues outlined the benefits of window of opportunity trials in publications in the Journal of Neurosurgery and Nature Medicine. "These trials not only generate improved pharmacokinetic and pharmacodynamic data but also help with the search for biomarkers and 'liquid biopsies'," Dr. Parney says.
Real-time assessments of treatment response
Synchronous data about tumor behavior is critical for monitoring a therapy's effectiveness in individual patients. "Gliomas adapt and evolve as a dynamic ecosystem. Biological feedback in real time from the tumor can help us stay ahead of disease," Dr. Burns says.
 肿瘤基本信息
肿瘤基本信息
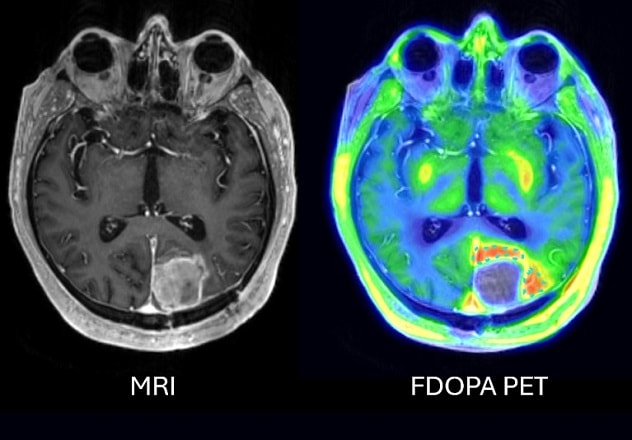
术后增强 MRI(左图)显示手术腔内有血液和液体,未见肿瘤增强。18F-DOPA 正电子发射体层成像(右图)显示,手术腔旁边的脑组织发生大量摄取,证实该区域有高级别胶质瘤残留。
To rapidly assess treatment response, neuroradiologists use not only MRI but also 18F-DOPA positron emission tomography (PET) to assess amino acid uptake.
"Although MRI provides vital information such as tumor location, 18F-DOPA PET imaging provides complementary information about physiological processes within a tumor," says Derek R. Johnson, M.D., chair of Nuclear Medicine at Mayo Clinic in Minnesota. "Amino acid PET imaging can sometimes identify tumor outside the areas suggested by MRI or clarify whether changes on MRI are due to tumor growth or treatment effect. Integrating MRI and 18F-DOPA PET imaging results gives the treatment team more information than can be obtained by either test alone."
Mayo Clinic specialists also analyze patients' blood and cerebrospinal fluid for tumor biomarkers. That information is then combined with the imaging results. Dr. Burns highlights the conceptual overlap between analyzing biomarkers and PET images and conducting a window of opportunity trial.
"Instead of performing a tissue biopsy, we're obtaining a liquid biopsy together with advanced imaging. These allow us to obtain more information at more timepoints than is typically plausible with tissue biopsies," he says. "More feedback means less guesswork and faster progress."
"Staying ahead of the tumor might require acting proactively — without waiting for tumor recurrence."
Targeting senescence
Standard-of-care chemotherapy and radiation kill only some tumor cells. The rest can enter stealth mode via a senescencelike state of mitotic arrest.
"Unfortunately, glioma cells don't stay inactive as long as we'd like. When they inevitably escape therapy-induced senescence, they can come back behaving more like stem cells that are especially difficult to control," Dr. Burns says.
As outlined by Mayo Clinic researchers in npj Precision Oncology, drugs that target senescent cells could help prevent tumor regrowth. "Staying ahead of the tumor might require acting proactively — without waiting for tumor recurrence," Dr. Burns says.
Mayo Clinic researchers have received approval for the first clinical trial of senolytic drugs for the treatment of glioma. The researchers are taking a new approach: iteratively testing multiple drugs in each patient within a single trial.
"We have seen only too well that the one-drug approach is woefully inadequate against glioma. If we see that a patient isn't responding to the current drug, we will switch quickly to the next drug in the algorithm," Dr. Burns says. "The goal is to add promising new drugs to this platform trial as they become available, without waiting for a new trial to start. Patients should always have the benefit of the best candidate drugs we have."
That commitment to patient care underlies Mayo Clinic's research efforts. "It's not just that the needs of the patient come first. Dr. William Mayo actually said, 'The best interest of the patient is the only interest to be considered,' " Dr. Burns says. "The fact that Mayo Clinic has been built around the needs of the patient empowers us to pursue out-of-the-box approaches that would be very difficult elsewhere. Our patients to us are like family. Their needs are why we're here and are 'the only interest to be considered.' "
For more information
Glioblastoma Therapeutics Network.
Parney IF, et al. The AANS/CNS Section on Tumors: A summary of 40 years of advocacy to advance the care of patients with brain and spine tumors. Journal of Neurosurgery. 2024;141:41.
Singh K, et al. Correcting the drug development paradigm for glioblastoma requires serial tissue sampling. Nature Medicine. 2023;29:2402.
Riviere-Cazeau C, et al. An untapped window of opportunity for glioma: Targeting therapy-induced senescence prior to recurrence. Precision Oncology. 2023;7:126.
Refer a patient to Mayo Clinic.