Jan. 23, 2021
微创肿瘤切除术
微创肿瘤切除术
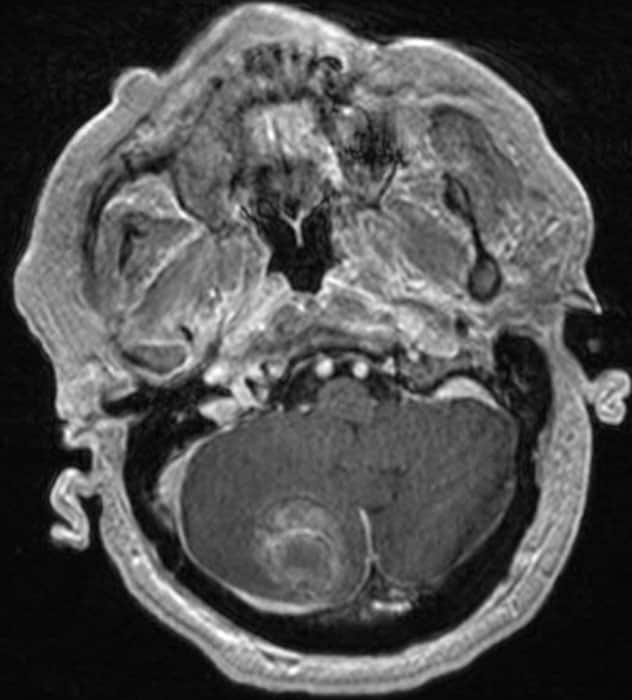
术前 MRI 显示大的小脑转移瘤。
颅骨钻孔切除术

颅骨钻孔切除术
通过尺寸小于 14 毫米的颅骨钻孔切除了大的小脑肿瘤。
术后影像学检查
术后影像学检查
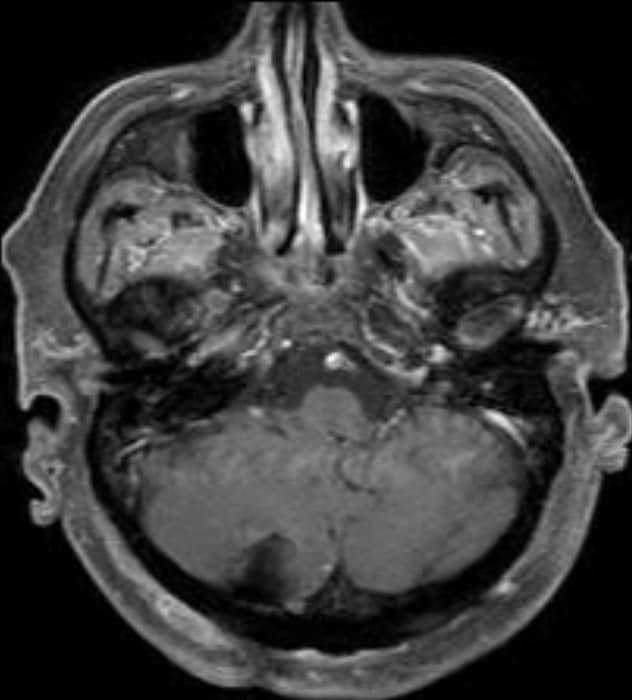
术后 MRI 显示大肿瘤完全切除。患者在术后第二天回家。
Mayo Clinic has successfully performed a series of intra-axial tumor resections using a burr hole approach with exoscopic visualization. The procedures, described in a study accepted for publication in the Journal of Neurological Surgery, provide proof of concept for this minimally invasive approach.
"This approach represents the extreme boundary of keyhole surgery. We have been able to resect select tumors through a 14-millimeter burr hole, similar to what is used for a needle biopsy," says Kaisorn L. Chaichana, M.D., a neurosurgeon at Mayo Clinic in Jacksonville, Florida. "Patients generally go home the following day and recover much faster."
Fourteen (93%) of the 15 patients in the Mayo Clinic study had gross total resection. The tumor remaining in one patient was minimal and subsequently resected. None of the 15 patients experienced complications after the burr hole procedure, and a majority went home the next day.
"The incision is very small — about three-fourths of an inch — and blood loss is much lower than with conventional surgery," Dr. Chaichana says.
Exoscopic visualization is the key to this approach. Compared with the endoscope, the exoscope provides a wider focus of view, greater magnification and oblique visualization angles.
"Our goal in this surgical series, as with all our patients, was to achieve maximal, safe resection," Dr. Chaichana says. "The exoscope, as opposed to the endoscope, hovers over the surgical field, not within the cavity. It provides a wider focus of view, greater magnification and oblique visualization angles that would be nonergonomic compared with the surgical microscope."
The burr hole approach is suitable for resecting superficial lesions. All tumors in the patients treated in the Mayo Clinic series were in close proximity to the cortical surface, with the most superficial part of the lesions located above the sulcal boundary in the coronal plane.
Patients with lesions presumed to be close to eloquent areas had functional MRI and diffusion tensor imaging before surgery. If access to the lesion required cortical or subcortical violation of eloquent areas, the burr hole approach wasn't used.
Among the patients studied, eight had metastatic brain tumors, four had low-grade glioma and three had high-grade glioma. Lesion diameter was typically limited to 4 centimeters. Dr. Chaichana notes that the burr hole procedure is also suitable for evacuating hematomas.
"A minimally invasive approach means patients heal faster, so they can start radiation and chemotherapy sooner, if needed," Dr. Chaichana says. "We believe the burr hole approach can be used for selective lesions without compromising the extent of resection or neurological outcomes."
For more information
Marenco-Hillembrand L, et al. Bur-hole based resections of intrinisic brain tumors with exoscopic visualization. Journal of Neurological Surgery. Part A, Central European Neurosurgery. In press.