July 30, 2022
Hyperglycemia is a common comorbidity in patients with Cushing syndrome (CS), with incidence ranging from 38% to 84%. While overall prevalence has been reported previously, details of the time course and the degree of postoperative improvement of this condition following curative surgery for CS have been limited overall.
To address this question, a retrospective study by Mayo Clinic Endocrinology, Diabetes, Metabolism, and Nutrition reviewed a large cohort of patients with various etiologies of CS who had curative surgery at Mayo Clinic between the years 2000 and 2019. The study team, — including six advanced practice providers with expertise in inpatient or outpatient diabetes mellitus management — published its results in the January 2022 edition of the Journal of the Endocrine Society.
Justine S. Herndon, P.A.-C., Endocrinology, Diabetes, Metabolism, and Nutrition, at Mayo Clinic in Rochester, Minnesota, and primary author of the study, says, "The idea for this study came from wanting to incorporate my work on our inpatient diabetes consulting service along with my outpatient work in pituitary and adrenal disorders. Often, on the inpatient side, when we see patients who are coming in for and achieve postsurgical remission of CS surgery, our diabetes management team might have difficulty with recommendations for postoperative glycemic control.
"We understand that with cure, hyperglycemia should improve, but we lacked understanding of the degree to which medication adjustment is necessary postoperatively as well as recommendations for outpatient follow-up. That led us to investigate glycemic changes within the first postoperative year and during glucocorticoid taper in this population. With the data we collected, we were able to do multiple analyses based on subtype and severity of CS and look further into diabetes medication changes and hemoglobin A1c (HbA1c) changes over time."
The cohort of 174 patients were identified as follows:
- 106 (60.9%) had CS
- 25 (14.4%) had ectopic CS
- 43 (24.7%) had adrenal CS or mild autonomous cortisol secretion
库欣综合征的手术缓解
库欣综合征的手术缓解
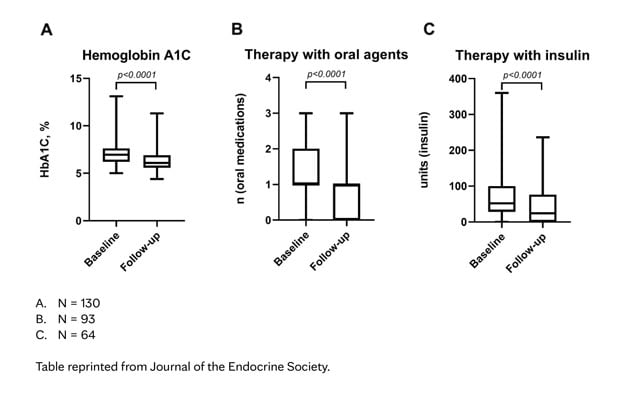
该表显示了 CS 手术缓解后基线和最后随访时,糖化血紅蛋白、口服药物数量和每日总胰岛素单位(长效、短效或中效)的时间线。
More than half of patients were determined to have severe CS based on biochemical or clinical severity scores. Most patients (76%) required medications (noninsulin and insulin therapies) for management of glucocorticoid-induced diabetes mellitus at baseline. Data about medication use were collected immediately postoperatively and at up to three various postoperative assessments within the first year, including a time when patients were weaning postoperative glucocorticoid replacement (if applicable). Median follow-up for this study was 10.5 months.
Irina Bancos, M.D., Endocrinology, Diabetes, Metabolism, and Nutrition, at Mayo Clinic in Rochester, Minnesota, explains, "Overall, we found that HbA1c levels decreased significantly over time by 0.84% when compared with baseline, and approximately two-thirds of patients had improvement or resolution in hyperglycemia." Her team defined this improvement as one of the following:
- Decrease in HbA1c or fasting glucose while on stable antihyperglycemic therapy
- Decrease in dose or number of antihyperglycemic medications or insulin by the treating provider if quantitative data such as HbA1c were not available (for example, reviewing patient logbooks)
Resolution or cure of hyperglycemia, defined as the absence of hyperglycemia (based on HbA1c or fasting glucose with review of patient's glucose log at the end of follow-up), was documented in 36 patients (21%). In patients taking oral agents alone, the number of medications to control hyperglycemia decreased by a mean of 0.5 agents from baseline (1.3 to 0.76 at follow-up, p ≤ 0.001).
Results
高血糖改善
高血糖改善
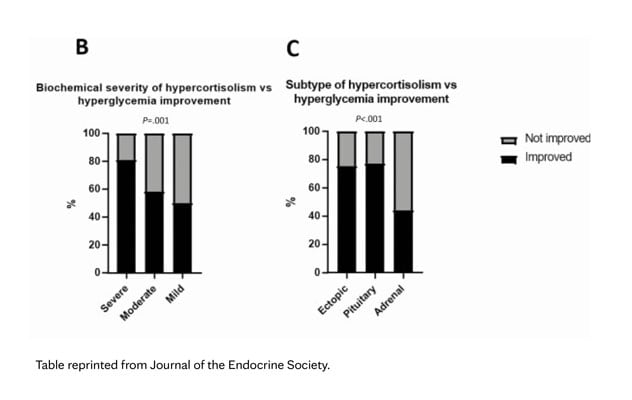
该表根据皮质醇增多症的严重程度和皮质醇增多症亚型显示高血糖改善。
In patients on insulin therapy, the total daily dose of insulin decreased by a mean of 30 units from baseline when accounting for patients who were able to discontinue insulin (72 units to 42 units at follow-up, p ≤ 0.001). The time frame of improvement and the decreased need for medication was seen over the entire study period, not just within the first three postoperative months. Notably, patients with higher degrees of CS severity (73 of 90 patients, 81.1%) and those with ACTH-dependent subtypes (99 of 129 patients, 76.7%) were statistically more likely to have improvement of hyperglycemia following CS remission. A small number of patients (17, 9.8%) required intensification of their hyperglycemia management in this study, and there were no statistically significant clinical or biochemical parameters that predicted this outcome.
In 137 patients (78.7%) with a documented BMI preoperatively and at follow-up, BMI decreased by a mean 3.16 kg/m2 from baseline (36.6 kg/m2 to 33.4 kg/m2). These findings were observed in 102 patients (58.6%) who were either no longer treated with glucocorticoids or reached a stable glucocorticoid replacement dose by the time of last follow-up.
As a result of this study, clinical recommendations are as follows:
- Patients with CS should be assessed for hyperglycemia preoperatively and treated accordingly.
- Anticipatory guidance should be given on the likelihood of decreased need for diabetes agents and dose requirements, especially for patients with severe CS or ACTH-dependent CS, as there is a statistically higher probability of improvement of hyperglycemia.
- Periodic but frequent follow-up after CS surgery should be conducted focusing on hyperglycemia with adjustments to medication regimens based on home glycemic control, fasting glucose levels and HbA1c levels, particularly in patients undertaking glucocorticoid tapers.
Conclusion
Herndon states, "Looping in other clinicians such as primary care providers and diabetes educators can be one way to fill the gap for busy endocrinology practices. Further prospective studies with specific follow-up protocols can reaffirm this data and provide even more concrete guidance on timeline for improvement and perhaps protocolized adjustments to hyperglycemia management postoperatively."
For more information
Herndon JS, et al. The effect of curative treatment on hyperglycemia in patients with Cushing syndrome. Journal of the Endocrine Society. 2022;6:1.
Refer a patient to Mayo Clinic.