Oct. 04, 2024
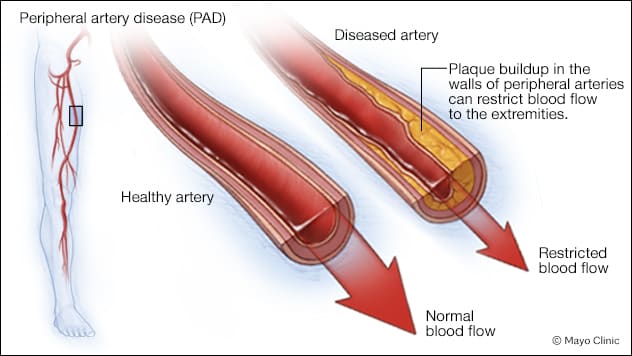 外周动脉疾病
外周动脉疾病
显示了血流正常的健康动脉和存在斑块堆积且血流受限的病变动脉。
 三维计算机体层成像扫描
三维计算机体层成像扫描
Shuja 医生与患者在检查室内讨论三维计算机体层成像扫描。
Mayo Clinic offers medical and surgical treatment for patients with peripheral artery disease (PAD), a chronic condition where plaque-related arterial narrowing reduces blood flow to the extremities. Patients' symptoms range from claudication to critical limb-threatening ischemia.
Fahad Shuja, M.B.B.S., a vascular surgeon at Mayo Clinic in Minnesota, says his interest in PAD was piqued due to its predominance in the population. PAD affects 10 million to 15 million individuals in the U.S. and 200 million to 250 million worldwide.
PAD risk factors and etiology
PAD rarely arises in isolation from other medical conditions, says Dr. Shuja. Over half the patients with PAD also have undiagnosed heart conditions, diabetes or failing kidneys.
"For patients with PAD, you're not just treating leg circulation," he says. "You're treating multiple organ systems."
Dr. Shuja says PAD is age related. It typically occurs in individuals in their 60s to 70s with a combination of cardiovascular risk factors, smoking, diabetes, high blood pressure or cholesterol, kidney disease, and heart disease.
This disease disproportionately affects specific societal segments: individuals in lower socioeconomic classes or Black people, Latinos and women. These groups also are more likely to present at an advanced PAD stage.
A disease with widely variable symptoms
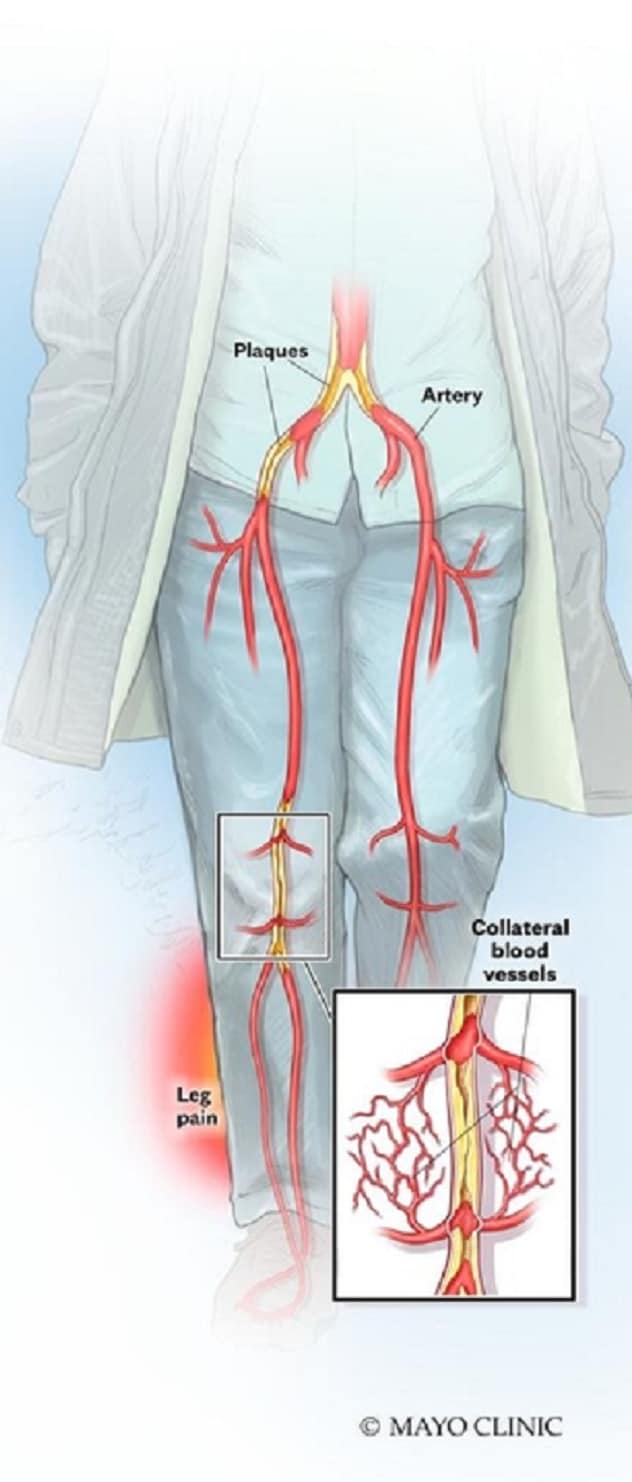 PAD 引起的腿部疼痛
PAD 引起的腿部疼痛
腿部动脉狭窄或阻塞引起腿部血流减少,从而导致腿部疼痛。
The variety of symptoms experienced with PAD complicates diagnosis. Some patients have no symptoms; others experience mild or pronounced symptoms, such as:
- Temperature changes. Coldness may arise in the lower leg or foot.
- Hip or leg muscle pain or cramping. Symptoms often begin with exercise and cease at rest, particularly after walking or stair climbing.
- Poor pulse. Patients may have a weak or undetectable pulse in the leg or foot.
Other PAD symptoms include:
- Leg skin color changes or shiny appearance.
- Slow-growing toenails.
- Unhealing sores in the toe, foot or leg.
- Leg hair loss or slowed growth.
- Erectile dysfunction.
- Limb-threatening extremity wounds and gangrene in advanced PAD.
First and second line PAD therapy
PAD treatment is lifelong, requiring continuous patient involvement for management.
"The more involved patients are, the more likely they'll have durable and successful treatment results; the process only works if patients take ownership of their health," says Dr. Shuja.
Dr. Shuja says a vascular surgeon does not address all a patient's PAD needs alone but with a multidisciplinary team.
"On average, patients with PAD meet 6 to 7 specialists at Mayo Clinic," he says. "This includes a vascular surgeon, dietitian, social worker, nicotine cessation counselor, diabetologist, wound care expert and cardiologist. Patients aren't just coming to Mayo Clinic to treat PAD — they're coming to treat the underlying reasons they developed PAD."
Dr. Shuja says a distinctive feature of Mayo Clinic PAD care is that these multidisciplinary professionals work under one roof.
"Patients don't have to walk across town to meet a dietitian, then drive 5 miles to meet a smoking cessation counselor," he says. "We bring the care professionals to them, making it easy to meet all these specialists."
Mayo Clinic PAD treatment begins with medical treatment to address PAD's root causes, including lifestyle changes. For those in the early stages, medical and lifestyle treatment alone can sometimes be sufficient. But for those with advanced stage, called critical limb-threatening ischemia, urgent revascularization is necessary to prevent an amputation.
For PAD treatment to work, it is vital that patients are involved from the beginning. They need to understand how they got PAD in the first place, what the potential complications are if it's not treated, and how individual therapies work.
Dr. Shuja also notes surgery cannot replace lifestyle changes.
"Surgery's not a substitute," he says. "It alone doesn't provide lasting benefits: It complements medical and lifestyle therapies and is needed when those don't suffice."
Surgery may involve minimally invasive options, such as balloon angioplasty and stent placement, or open surgery, such as endarterectomy or a bypass operation. Mayo Clinic vascular surgeons offer both these options.
He tells patients that the Mayo Clinic team will treat not only the patient's PAD but also its causes and provide resources for a durable, sustainable outcome.
Mayo Clinic also focuses on PAD research, which supports clinical care. Mayo Clinic is one of a few centers nationally studying laboratory-developed arteries for patients who lack bypass-suitable veins as part of a clinical trial. Furthermore, Dr. Shuja has been working on a human tissue bank of plasma and arteries from patients with PAD to study the disease's biology. He says the goal is to detect PAD early and develop more effective medical PAD treatments.
When to refer patients with PAD
When patients have leg pain with exertion and weak or absent pulses in the leg, Dr. Shuja recommends referring them to a specialty vascular center such as Mayo Clinic in Minnesota. Referral needs increase if these risk factors are present:
- Diabetes.
- Family history of PAD, stroke or heart attack.
- High blood pressure or cholesterol.
- Increased age, especially 65-plus, or 50-plus for patients with atherosclerosis risk factors.
- Obesity.
- Smoking.
"Untreated PAD's biggest risk is limb loss, which causes loss of independence. What limb loss means for patients is unimaginable — one of the most life-changing moments for that patient."
Dr. Shuja suggests prompt referral due to potential severe PAD atherosclerosis-related complications, including:
- Critical limb-threatening ischemia. This condition often presents with open, unhealing limb sores or gangrene. Untreated, critical limb-threatening ischemia leads to leg amputation in up to 40% of patients.
- Stroke and heart attack. Arterial plaque buildup may affect the blood vessels of the heart or brain.
"Untreated PAD's biggest risk is limb loss, which causes loss of independence," he says. "What limb loss means for patients is unimaginable — one of the most life-changing moments for that patient.
"Only pancreatic cancer has a shorter life expectancy than critical limb-threatening ischemia, the severe form of PAD," says Dr. Shuja. "This is a deadly disease because it's a marker of overall cardiovascular health. I can't say enough about how important it is to care for PAD."
Dr. Shuja says his team does not need to repeat local testing. They spend time working with hometown physicians to understand the testing, workup and treatments the patient has already undergone. When a patient is referred to Mayo Clinic, the team works to coordinate all the patient's appointments in a short time frame.
For more information
Refer a patient to Mayo Clinic.