Overview
Radiation therapy
Radiation therapy
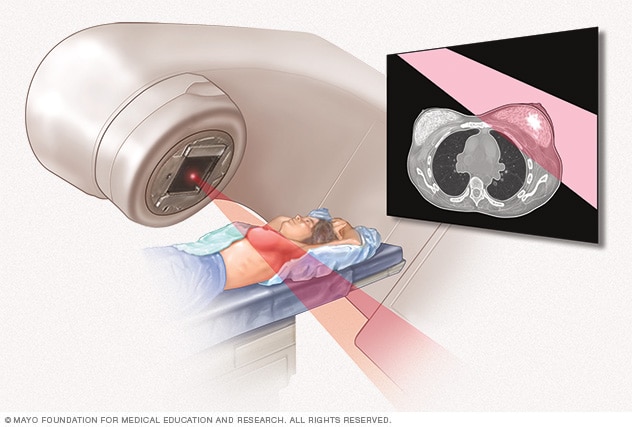
External beam radiation uses high-powered beams of energy to kill cancer cells. Beams of radiation are precisely aimed at the cancer using a machine that moves around your body.
Radiation therapy, also called radiotherapy, is a type of cancer treatment. This treatment uses beams of intense energy to kill cancer cells. Radiation therapy most often uses X-rays. But other types of radiation therapy exist, including proton radiation.
Modern methods of radiation are precise. They aim beams directly at the cancer while protecting healthy tissues from high doses of radiation.
Radiation therapy can be given inside or outside of your body. The most common kind is external beam radiation therapy. This treatment uses a large machine called a linear accelerator. High-energy beams are aimed from the machine to a precise point on your body.
Radiation treatment that goes inside the body is called brachytherapy (brak-e-THER-uh-pee). Brachytherapy also is a common cancer treatment. During this therapy, a provider places a small solid implant in or near the cancer.
Radiation therapy damages cells by destroying their genetic material. Genetic material controls how cells grow and divide. Healthy cells may be damaged along with cancer cells during radiation therapy. But healthy cells can repair themselves more easily than cancer cells. The goal of the radiation therapy is to treat the cancer while harming as few healthy cells as possible.
Why it's done
Radiation therapy is used to treat just about every type of cancer. In fact, more than half of all people with cancer will receive radiation therapy as part of their treatment. Radiation therapy also may be used to treat some conditions that aren't cancerous. This includes tumors that aren't cancerous, called benign tumors.
How radiation therapy is used in people with cancer
Radiation therapy might be used at different times or for different reasons during your cancer treatment.
Your care team may suggest radiation:
- As the only treatment for cancer. This is called the primary treatment.
- Before surgery, to shrink a cancer. This is called neoadjuvant therapy.
- After surgery, to stop the growth of any remaining cancer cells. This is called adjuvant therapy.
- With other treatments, such as chemotherapy, to destroy cancer cells.
- To relieve symptoms caused by advanced cancer.
Risks
You may or may not have side effects from radiation therapy. It depends on which part of your body is getting the radiation and how much is used. If you do have side effects, they can be controlled during treatment. After treatment, most side effects will go away.
| Part of body being treated |
Common side effects |
| Any part |
Hair loss at treatment site (sometimes permanent), skin irritation at treatment site, fatigue |
| Head and neck |
Dry mouth, thickened saliva, difficulty swallowing, sore throat, changes in the way food tastes, nausea, mouth sores, tooth decay |
| Chest |
Difficulty swallowing, cough, shortness of breath |
| Abdomen |
Nausea, vomiting, diarrhea |
| Pelvis |
Diarrhea, bladder irritation, frequent urination, sexual dysfunction |
Sometimes side effects develop after treatment. These are called late side effects. Very rarely, a new cancer may develop years or decades after cancer treatment. It can be caused by radiation or other treatments. This is called a second primary cancer. Ask your provider about any side effects that could happen after treatment, both short term and long term.
How you prepare
Before external beam radiation therapy, you will meet with a doctor who specializes in using radiation to treat cancer. This doctor is called a radiation oncologist. Together you can consider whether radiation therapy is right for you.
If you decide to move forward, your care team will carefully plan your treatment. They'll find the exact spot on your body to make sure the right amount of radiation goes where it's needed. Planning typically includes:
-
Radiation simulation. During simulation, your radiation therapy team will help you find a comfortable position. You must lie still during treatment, so being comfortable is important.
To practice, you'll lie down on the same type of table that will be used during your treatment. Cushions and props will help hold you in the right way so you can be still. You might be fitted for a body mold or mesh face mask to help keep you in place.
Next, your radiation therapy team will mark the place on your body that will get the radiation. This might be done with a marker or with small permanent tattoos. It all depends on your situation.
- Planning scans. Your radiation therapy team will use scans to map out your custom radiation plan. These might include CT scans or MRIs. During these scans, you will lie in the treatment position wearing the mask or mold made for you.
After planning, your care team will decide the type and dose of radiation you'll get. This is based on the kind of cancer you have, your general health and goals for your treatment.
Planning is important to get the dose and focus of the radiation beams right. When this is precise, there is less harm to healthy cells around the cancer.
What you can expect
External beam radiation therapy

External beam radiation therapy
During external beam radiation therapy, you lie on a table. A large machine moves around you, sending beams of radiation into precise points in your body.
External beam radiation therapy uses a machine that aims high-energy beams into your body. This is called a linear accelerator.
As you lie still, the linear accelerator moves around you. It delivers radiation from several angles. The machine is adjusted just for you by your care team. That way, it delivers the precise dose of radiation to the exact point on your body. You will not feel the radiation as it is being delivered. It is like getting an X-ray.
External beam radiation is an outpatient treatment. This means you won't need to stay in the hospital after treatment. It's common to get therapy five days a week over several weeks. Some treatment courses are given over 1 to 2 weeks. The treatment is spread out this way so that healthy cells have time to recover between sessions. Sometimes only one treatment is used to relieve pain or other symptoms from more advanced cancers.
Expect each session to last about 10 to 30 minutes. Most of that time is spent getting your body in the right position. During treatment, you'll lie on the table in the same way you did during planning. The same molds and props might be used to help hold you in place.
The linear accelerator machine makes a buzzing sound. Also, it may rotate around your body to reach the target from different angles.
Your radiation therapy team stays in a room nearby. You'll be able to speak to them through video and audio connecting your rooms. Although you shouldn't feel any pain from the radiation, do speak up if you feel uncomfortable.
Results
After radiation therapy, you might have imaging tests to see if the cancer is shrinking. Sometimes the cancer responds to treatment right away. Other times it may take weeks or months to see the treatment working. Ask your radiation therapy team what you can expect.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.