April 23, 2019
Female pelvic floors disorders are highly prevalent, with up to 25 percent of women having one or more ― such as urinary incontinence, pelvic organ prolapse or genitourinary fistulae. In fact, in women, the lifetime risk of undergoing surgery for pelvic organ prolapse or stress urinary incontinence by age 80 is roughly 20 percent.
Mayo Clinic offers a unique, multidisciplinary approach to managing these sensitive conditions: Collaboration among urologists, gynecologists and colorectal surgeons allows for individualized decision-making and broad access to a multitude of treatment options.
Vaginal colporrhaphy
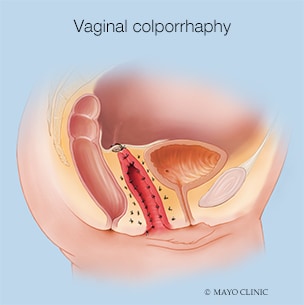
Vaginal colporrhaphy
Treatment options available for patients with pelvic organ prolapse include surgeries via vaginal, abdominal or robotic approaches.
In managing pelvic organ prolapse, treatment options range from observation to pessary use or surgeries via vaginal, abdominal or robotic approaches. Depending on the individual patient, surgical procedures for pelvic organ prolapse may include use of a patient's own tissue (native-tissue repair), use of polypropylene mesh, and hysterectomy.
By having specialized surgeons dedicated to treating women with pelvic organ prolapse, Mayo Clinic has developed a high-volume practice with each of the various surgical approaches. "Each management option possesses a unique blend of risks and benefits, and we strive for shared decision-making with our patients to make sure their treatment goals are attained," says Brian J. Linder, M.D., a urologist with a joint appointment in Urology and Obstetrics and Gynecology who specializes in female pelvic medicine and reconstructive surgery at Mayo Clinic's campus in Rochester, Minnesota.
Open versus minimally invasive sacrocolpopexy
Sacrocolpopexy with mesh
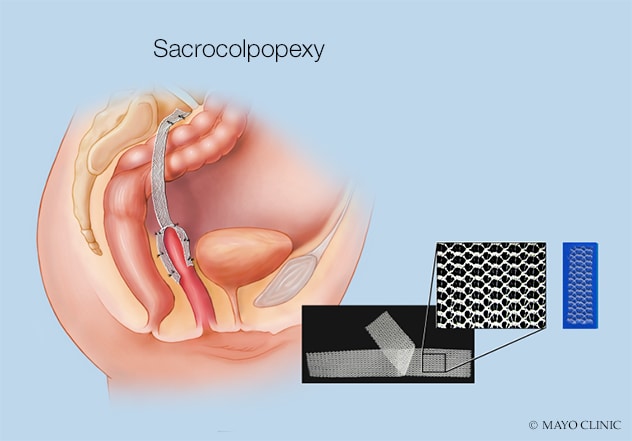
Sacrocolpopexy with mesh
Surgical procedures for pelvic organ prolapse may include native-tissue repair, use of polypropylene mesh and hysterectomy.
Dr. Linder is particularly interested in the safety and efficacy of pelvic organ prolapse repairs. Along with colleagues in both Urology and Obstetrics and Gynecology, he authored a manuscript in the Journal of Urology that sought to assess the perioperative outcomes of minimally invasive and open sacrocolpopexy.
The National Surgical Quality Improvement Program was accessed to conduct the study. The percentage of cases performed with a minimally invasive approach increased from 70 percent in 2010 to 82 percent in 2016. Importantly, minimally invasive sacrocolpopexy was found to have a reduced risk of complications, need for blood transfusion, prolonged hospitalization and readmission. Mayo Clinic has a robust practice that incorporates minimally invasive ― such as robotic ― sacrocolpopexy in appropriate patients.
Likewise, the management of urinary incontinence is largely based on patient treatment preferences. For instance, several more-advanced treatments are offered to patients who have been unsuccessful in managing overactive bladder symptoms (urinary urgency, frequency or incontinence) with more conservative measures. Depending on the clinical scenario, patients have access to therapies such as sacral neuromodulation, percutaneous tibial nerve stimulation or bladder onabotulinumtoxinA injection. Each of these therapies is minimally invasive, with onabotulinumtoxinA injection and tibial nerve stimulation performed in the office setting.
For management of stress urinary incontinence, both mesh- and non-mesh-based procedures are available. In addition, a unique collaboration with Colon and Rectal Surgery is available for the management of concomitant pelvic organ prolapse and rectal prolapse, allowing both conditions to be treated during a single surgery.
For more information
Linder BJ, et al. A national contemporary analysis of perioperative outcomes of open versus minimally invasive sacrocolpopexy. Journal of Urology. 2018;200:862.
To refer a patient to Mayo Clinic's multidisciplinary female pelvic floor clinic, visit Medical Professionals Provider Relations.