Dec. 21, 2023
Radiation therapy for prostate cancer, while curative, is not without its associated side effects. The targeted destruction of cancerous cells can inadvertently impact surrounding healthy tissue, leading to various adverse effects. Common side effects include urinary problems such as increased frequency, urgency and discomfort during urination.
Radiation-induced membranous urethral stricture is a less common but challenging complication. Nick Warner, M.D., a urologist at Mayo Clinic in Rochester, Minnesota, is developing a technique to treat these challenging strictures without incisions.
Membranous urethral stricture
The membranous urethra is part of the urethra that drains the male bladder. The membranous urethra is the section of the urethra that runs through the pelvic muscles. A narrowing at this location is known as a membranous urethral stricture. This is a result of damage to the tissue due to primary or salvage radiation. Regardless of the cause, the stricture poses a hurdle due to its intricate connection with pelvic muscles and the continence mechanism in men, especially when the prostate has been previously removed.
Membranous urethra work-up
Cystoscopy. A physician passes a camera through the urethra into the bladder to inspect the location of the narrowing. This is a crucial step to make sure the narrowing is at the membranous urethra. It is important to do cystoscopy while patients are awake so that they can perform contractions of the pelvic floor while the physician investigates.
Voiding cystourethrogram. An X-ray of the bladder and urethra after the bladder has been filled with contrast is taken. This is not required in all patients, but it can be helpful if the narrowing is very tight.
Uroflow. The strength of the urine stream is measured.
International Prostate Symptom Score. This questionnaire helps healthcare professionals better understand and rate symptom severity.
Treatment and management techniques
Various management strategies exist for membranous urethral strictures, each presenting distinct considerations. One approach involves self-catheter dilation, a daily routine aimed at maintaining urethral patency. However, this approach has potential drawbacks such as pain and recurring urinary tract infections. It also limits the ability to address concurrent urinary incontinence.
Another option is the excision and primary anastomosis technique. During this treatment, a physician removes scar tissue and rejoins the urethra. This surgery is often performed through incisions behind the scrotum and lower abdomen, in some cases with the aid of robotic surgery.
Despite these treatment options, postoperative incontinence — particularly after the prostate has been previously removed — remains a common challenge due to the intricate connection with the continence mechanism. In addition, given the need to mobilize the urethra, future surgeries to correct incontinence can be more difficult. Alternatively, grafting the narrow segment of the urethra with tissue from the oral cavity presents a method with less urethral mobilization and potential benefits for future anti-incontinence procedures. This technique also can be challenging given the depth of the graft deployment.
 Endoscopic buccal mucosal grafting
Endoscopic buccal mucosal grafting
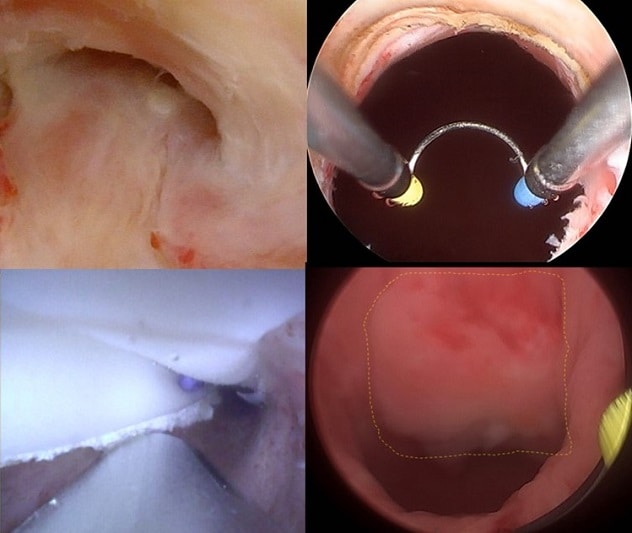
This image shows the membranous urethral stricture (upper left); resection of the strictured urethra (upper right); buccal graft deployment (lower left); and healed graft at the four-month cystoscopy (lower right).
Dr. Warner's minimally invasive technique, recently presented at the American Urological Association (AUA) annual meeting and published in a 2023 issue of Urology, involves cystoscopy, dilation, scar tissue resection, graft deployment and catheter placement. This technique has yielded promising results in terms of urethral patency and patient outcomes.
This method circumvents the need for scrotal incisions, reduces operative time and facilitates future anti-incontinence procedures. Follow-up on patients, many now exceeding one year after surgery, has revealed favorable voiding outcomes in the majority, showcasing the potential advantages of this approach.
For more information
Ungerer G, et al. Endoscopic urethroplasty using buccal graft for male membranous urethral stricture. Urology. 2023;181:e200.
Refer a patient to Mayo Clinic.