July 14, 2022
Pediatric idiopathic tracheal stenosis (PITS) is an extremely rare disease generally occurring before puberty in children without other underlying conditions. The disease arises from an unknown etiology and creates a spiral idiopathic stenosis of the trachea. The affected area can be focal, or the disease may impact multiple areas of the trachea.
While the cause of the disease is unknown, it may arise after an upper respiratory infection or a traumatic event such as intubation. Biopsy of affected tissue may show eosinophils, but scar tissue is the predominant finding.
The pediatric aerodigestive program at Mayo Clinic Children's Center is unique in that it provides comprehensive diagnostic and treatment services for patients with PITS through its multidisciplinary team approach. Treatment takes place in two stages.
After patients are referred to Mayo Clinic, they first undergo a complete diagnostic evaluation to assess the airway, establish the extent of the disease, and rule out other underlying conditions, such as reflux or other inflammatory diseases.
Joshua P. Wiedermann, M.D., a pediatric otorhinolaryngologist at Mayo Clinic Children's Center at Mayo's campus in Rochester, Minnesota, says, "We pride ourselves on crafting an entire program for our visiting patients so that we can figure out what questions need to be answered. We gather all the data and diagnostic information and then perform corrective surgery if needed."
The multidisciplinary team is headed by R. Paul Boesch, D.O., a pediatric pulmonologist at Mayo Clinic in Minnesota, and includes experts in pulmonology, otolaryngology, gastroenterology, speech therapy, sleep medicine and other relevant experts.
Tracheal wedge excision
Tracheal wedge excision
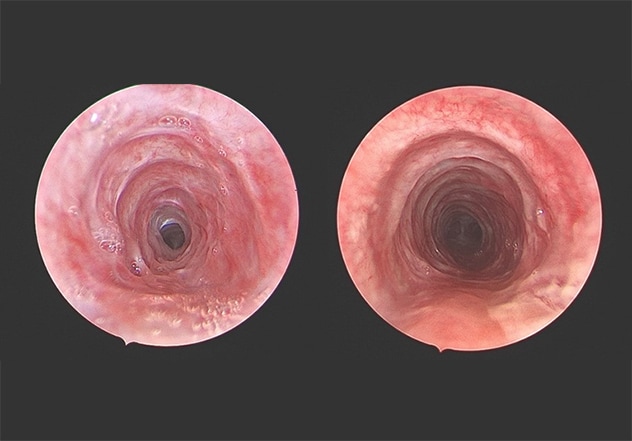
Before and after tracheal wedge excision (6 months apart) in a 12-year-old with PITS.
The interdisciplinary team then provides an innovative treatment called tracheal wedge excision that includes both surgical and medical components. Surgical treatment involves carbon dioxide laser scar excisions as an alternative to traditional endoscopic balloon dilation that may propagate the spread of the disease.
In the wedge excision procedure, large wedges of stenotic tissue are excised while preserving small bridges of tissue to allow for re-mucosalization and prevent circumferential scarring. Mayo Clinic clinicians have performed the procedure in adults for over two decades, and initial findings — published in a 2021 issue of Laryngoscope — demonstrate increased time between surgeries compared with standard laser and balloon dilation.
Mayo Clinic Children's Center is the first location to use tracheal wedge excision in pediatric patients. After excision, patients are treated with antibiotics, inhaled corticosteroids and proton pump inhibitors for several months. Follow-up with the multidisciplinary team takes place 3 to 6 months later, and thus far, patients have experienced complete resolution of their symptoms.
Due to the rarity of PITS among the general pediatric population, affected patients can benefit from the expertise and multidisciplinary approach that Mayo Clinic provides. Another unique aspect of the Mayo Clinic Children's Center aerodigestive program is the way experts integrate 3D printing technology with airway reconstruction.
"When we have patients who need airway reconstruction, we partner with our 3D anatomy team, which can take images from CT scans and create high-fidelity 3D models," Dr. Wiedemann explains. "They can be cut, manipulated and sutured, so we can practice the surgery multiple times before going into the procedure."
For more information
Mayo Clinic Children's Center.
Ekbom DC, et al. Endoscopic wedge excisions with CO2 laser for subglottic stenosis. Laryngoscope. 2021;131:E1062.
Refer a patient to Mayo Clinic.