Sept. 06, 2018
Pediatric patients with congenital heart disease can have complex medical issues and may eventually need heart transplantation. A true multidisciplinary approach and expertise in the transition to adult care are required when treating these challenging cases. At Mayo Clinic's campus in Rochester, Minnesota, pediatric cardiologists work with pediatric practitioners in other specialties, as well as specialists in adult care, to treat patients with congenital heart disease.
"The great strength of our practice is the multidisciplinary care — multiple people working together when we see kids with complex medical problems," says Jonathan N. Johnson, M.D., a pediatric cardiologist at Mayo Clinic. "When a 16-year-old comes in with autoimmune myocarditis, one of the world's experts in that condition is down the hall from me. It's easy for me to pick up the phone, and 15 minutes later that physician is seeing the patient with me."
Prenatal to adult care
Mayo Clinic's comprehensive approach encompasses a full range of echocardiography services, including transthoracic and transesophageal echocardiograms, as well as fetal echocardiography when a fetal heart abnormality is suspected. Diagnosing conditions such as hypoplastic left heart syndrome before birth allows physicians to plan the safest possible birth and postnatal treatment.
As a primary center for children and adults, Mayo Clinic offers treatment for congenital heart defects as the patient's condition progresses through childhood and into adulthood. Children and adults needing heart transplantation are treated at the Mayo Clinic Transplant Center, which has both pediatric and adult cardiologists and nurses.
"When our transplant patients transition to adult care, they don't move to a different clinic," Dr. Johnson says. "The only thing that changes is the doctor. We even have the same nurse coordinator working with these patients as children and as adults. The process is as seamless as it can be."
Chest radiographs before and after heart transplantation
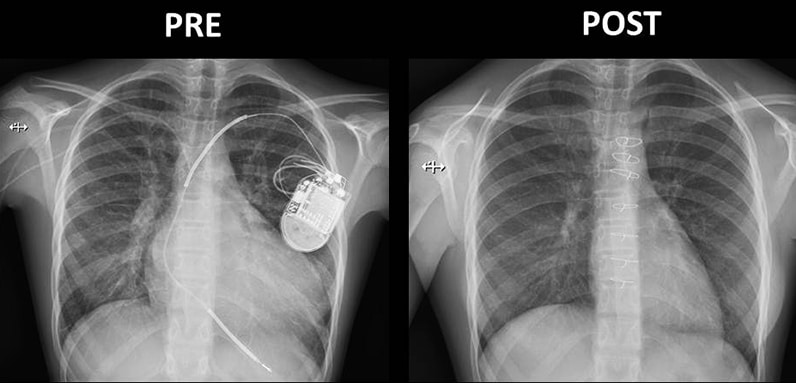
Chest radiographs before and after heart transplantation
On the left, chest radiograph shows damage to the heart of an 11-year-old girl with severe dilated cardiomyopathy. An implantable cardioverter defibrillator and a peripherally inserted central catheter for delivering intravenous milrinone infusion are visible. On the right, radiography shows the same patient's chest after heart transplantation.
The latest technology is available for treating pediatric patients, including pediatric ventricular assist devices for children with heart failure who are awaiting transplant. "Our knowledge of how best to utilize these devices in pediatric patients continues to grow," Dr. Johnson says.
Heart transplantation
Pediatric heart transplant 1982-2017 outcomes
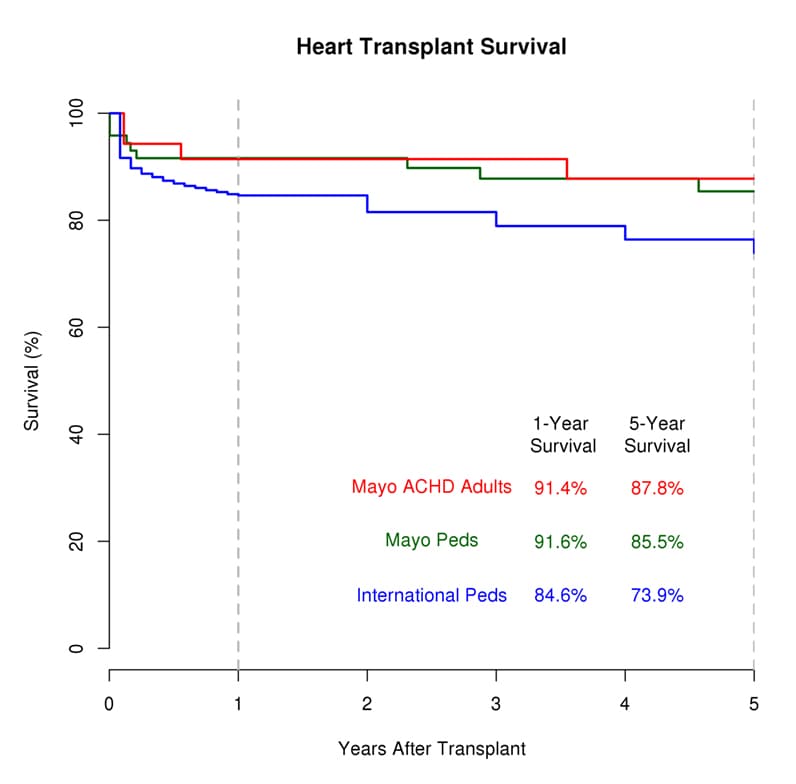
Pediatric heart transplant 1982-2017 outcomes
At Mayo Clinic, one-year and five-year survival rates after heart transplantation for congenital heart defects exceed the international average. Outcomes for pediatric patients and patients with adult congenital heart disease (ACHD) at Mayo Clinic are shown in red; pediatric patients at Mayo Clinic, in green. Blue indicates international outcomes as reported by the International Society for Heart and Lung Transplantation.
Every year, Mayo Clinic performs eight to 10 heart transplants in children and in adults with congenital heart defects. Heart transplant outcomes exceed the national average.
According to a retrospective study, published in the April 2014 issue of Mayo Clinic Proceedings, of all patients with congenital heart disease who underwent heart transplantation at Mayo Clinic's campus in Minnesota from 1990 to 2012, patient survival at one, five and 10 years was 89 percent, 89 percent and 72 percent, respectively, exceeding national results over the same time frame. Of the 45 patients studied, only six patients (13 percent) had no previous cardiac operation; the remaining 39 patients had a mean of three previous cardiac surgeries.
Three patients in the study underwent combined heart-liver or combined heart-kidney transplant. Failure of a second organ system is a notable issue in many patients with congenital heart disease. Although complex multiorgan transplants have typically been reserved for adults, Mayo has begun performing these procedures in pediatric patients. The first pediatric combined heart-kidney transplant at Mayo Clinic was performed in 2012, in a 12-year-old boy. In 2014, the first pediatric combined heart-lung transplant at Mayo Clinic was performed in a 13-year-old girl.
Novel immunosuppression approach
Mayo Clinic has an innovative protocol for immune suppression in pediatric transplant patients involving, when appropriate, novel drugs including sirolimus — a drug used increasingly in adult transplant patients who experience nephropathy from calcineurin inhibitor (CNI) drugs. Sirolimus generally hasn't been used as a first line immunosuppressant in pediatric heart transplant patients. However, a Mayo Clinic study published in the December 2013 issue of Pediatric Transplantation found beneficial effects from that treatment.
The researchers reviewed the records of 20 patients for whom conversion to a CNI-free, sirolimus-based regimen was attempted. Sixteen patients were successfully converted; follow-up was available for a mean 2.5 years after conversion. The rate of rejection while taking CNIs was 0.18 rejections per patient-year compared with 0.03 rejection episodes per patient-year while on sirolimus. Renal function, measured by glomerular filtration rate, significantly improved after sirolimus conversion.
Six of 20 patients (30 percent) experienced adverse effects from conversion to sirolimus. The researchers note concerns with patient tolerability and the need for larger and more long-term studies. "But renal insufficiency and subsequent renal replacement therapy are major morbidities in pediatric heart transplant patients nationally," Dr. Johnson says. "We think this new immunosuppressive regimen offers great potential for our patients."
Regenerative medicine
An additional option in the future for certain patients with congenital heart disease may include stem cell therapies. Mayo Clinic is conducting the first stem cell clinical trial in the U.S. for pediatric patients with congenital heart disease. The trial focuses on the safety and feasibility of using autologous stem cells to treat children with hypoplastic left heart syndrome. The stem cells, collected from the patient's umbilical cord following birth, will be injected into the patient's heart muscle during the second surgical treatment for hypoplastic left heart syndrome, which is typically performed at ages 4 to 6 months.
"Our pediatric cardiology practice has direct links to the Mayo Clinic Center for Regenerative Biotherapeutics. Stem cell-based regeneration may potentially help these children to grow stronger hearts, and avoid heart transplantation," Dr. Johnson says. "It's that richness of connections to colleagues throughout Mayo Clinic that we can offer our patients."
For more information
Robinson JA, et al. Cardiac and multiorgan transplantation for end-stage congenital heart disease. Mayo Clinic Proceedings. 2014;89:478.
Loar RW, et al. Empiric switch from calcineurin inhibitor to sirolimus-based immunosuppression in pediatric heart transplantation recipients. Pediatric Transplantation. 2013;17:794.
The Journal of Heart and Lung Transplantation. The Registry of the International Society for Heart and Lung Transplantation: Twenty-seventh official adult heart transplant report — 2010. 2010;29:1104.
Safety Study of Autologous Umbilical Cord Blood Cells for Treatment of Hypoplastic Left Heart Syndrome. Mayo Clinic.