March 20, 2018
Surgical site infection is a challenging complication associated with total joint arthroplasty.
Although infection is relatively uncommon, the number of infections is rising as total hip arthroplasty and total knee arthroplasty are increasingly performed on an aging population. As a major referral center, Mayo Clinic has significant experience and expertise treating these prosthetic joint infections.
"We have sufficient patient volume that we are able to offer patients a surgeon who focuses on these types of cases. Treating these joint infections accounts for a large part of my practice," says Kevin I. Perry, M.D., a consultant in Orthopedic Surgery at Mayo Clinic in Rochester, Minnesota.
Anteroposterior radiograph showing articulating antibiotic spacer

Anteroposterior radiograph showing articulating antibiotic spacer
Anteroposterior radiograph shows an articulating antibiotic spacer used for an infected total hip arthroplasty.
Lateral radiograph showing articulating antibiotic spacer
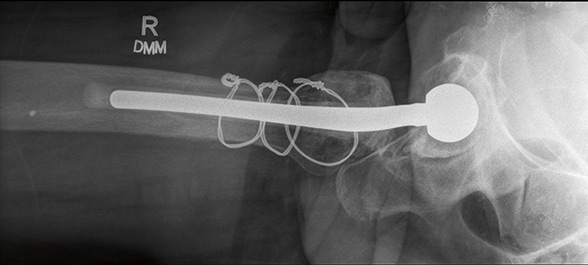
Lateral radiograph showing articulating antibiotic spacer
Lateral radiograph shows an articulating antibiotic spacer used for an infected total hip arthroplasty.
Through the use of antibiotic spacers fabricated at the time of surgery, Mayo Clinic is able to provide patients with maximal use of their joints during treatment. "These types of spacers allow patients reasonable function during the treatment period. As a result, many patients are able to put weight on the joint and to move around while we clear the infection," Dr. Perry says.
Treating joint infections is complex, requiring open surgery to remove the patient's prosthetic, thorough debridement of the infected material and insertion of the antibiotic spacers. Patients then typically have a six-week course of intravenous antibiotics and, after a period of waiting to ascertain that the infection has cleared, a second open procedure to remove the spacers and replace the prosthetic.
"The great strength we have at Mayo Clinic is coordination of care," Dr. Perry says. "As orthopedic surgeons, we work very closely with subspecialists in orthopedic infectious diseases. Often the orthopedic surgeon and the orthopedic infectious disease specialist see the patient together. We have a good working relationship to come up with the best plan to treat these patients."
At Mayo Clinic, most joint infections are cleared completely. "Outcomes depend a lot on the health of the patients — their medical comorbidities, the number of operations they've had and the status of the infected limb," Dr. Perry says. "But in generally healthy patients, we see a better than 90 percent cure rate."
Underpinning this clinical practice is a research program focused on improving treatment for patients with prosthetic joint infections. In a study published in the November 2017 issue of The Journal of Arthroplasty, Mayo Clinic researchers found that prolonged retention of an antibiotic spacer — which is occasionally chosen in treatment of a hip or knee infection if the patient is considered medically unfit for future surgery — leads to frequent mechanical failure and relatively poor clinical outcomes.
"We've learned to control the surgical and postoperative environments to minimize the risk of infection," Dr. Perry notes. "But because the number of arthroplasty procedures continues to rise, infection will continue to be a burden."
For more information
Petis SM, et al. Retained antibiotic spacers after total hip and knee arthroplasty resections: High complication rates. The Journal of Arthroplasty. 2017;32:3510.