July 20, 2021
Central retinal artery occlusion and branch retinal artery occlusion (collectively referred to as retinal artery occlusion or RAO) are analogous to an acute stroke of the brain or heart — and may be a harbinger of a central nervous system stroke. RAO commonly occurs as a result of an embolic event in the context of carotid artery plaque. Various features of carotid plaque increase the risk of ischemic cerebral events, including ulceration, inflammation, neovascularization and degree of stenosis.
Retinal artery occlusion
Retinal artery occlusion
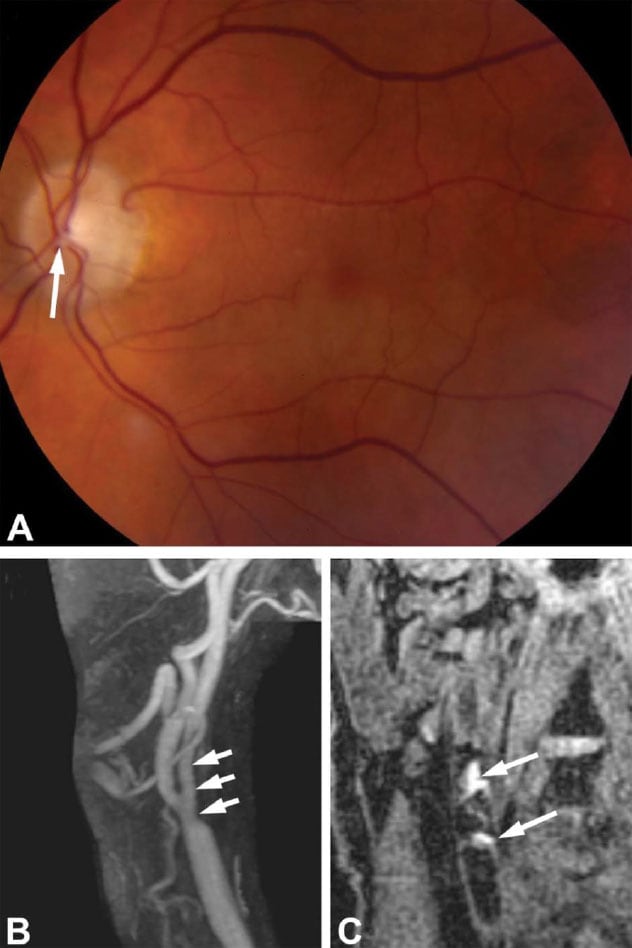
Retinal artery occlusion in the setting of ipsilateral carotid intraplaque hemorrhage with minimal stenosis. An older adult male with a history of coronary artery disease and hypercholesterolemia presented with sudden painless vision loss in the lower left visual field. The patient did not have any other neurological symptoms. A. Fundus photograph demonstrates a plaque in the inferior arcade coming off the disk (arrow) with inferior retinal whitening consistent with a hemiretinal artery occlusion in the left eye. Echocardiography and Holter monitoring did not show any evidence of cardiac structural abnormalities or arrhythmias. B. Magnetic resonance angiography shows long segment irregularity of the left internal carotid artery (arrows) but less than 50% stenosis. C. Magnetization prepared-rapid gradient echo protocol for detection of plaque hemorrhage shows T1 hyperintense plaque of the right carotid bifurcation suggesting intraplaque hemorrhage (arrows). The patient was treated with aspirin and a statin and did not experience any new ocular or neurological symptoms at 23-month follow-up. Image reprinted with permission from Journal of Neuro-Ophthalmology.
"Recently, plaque imaging with various sequences on high-resolution magnetic resonance vessel wall imaging has enabled detection of intraplaque hemorrhage (IPH), which been associated with an acceleration in plaque progression and an increased risk of plaque rupture. Intraplaque hemorrhage has also been shown to be predictive of future cerebral ischemic events," says Muhammad (M. Tariq) T. Bhatti, M.D., a neuro-ophthalmologist at Mayo Clinic in Rochester, Minnesota. "However, whether such an association between carotid IPH and RAO exists remains unknown. If it does exist, it would emphasize the importance of examining for the presence of IPH on high-resolution magnetic resonance angiography (HR-MRA) of the cervical carotid arteries in the setting of acute retinal ischemia."
Dr. Bhatti and his fellow researchers in Radiology, Neurology and Neurosurgery sought to test whether that association does exist. Their study was published in the Journal of Neuro-Ophthalmology in 2021.
The team requested medical and imaging records of all patients who underwent neck MRA with plaque imaging that included high-resolution vessel wall imaging with magnetization prepared-rapid gradient echo sequences at Mayo Clinic between 2015 and 2020. From the 643-member cohort, 14 patients were identified who had ophthalmologically confirmed RAO and HR-MRA plaque imaging of the neck performed within six weeks after an acute retinal ischemic event.
For comparison, 211 patients who had neck MRA with magnetization prepared-rapid gradient echo sequences performed but did not have a history of a cerebral ischemic event were identified and used as controls.
Data collected included demographic information such as patient age, sex and body mass index from the medical records of included patients. The researchers also noted the presence of comorbid conditions and collected values of laboratory studies.
Dr. Bhatti notes: "There was a higher prevalence of males in the RAO group (78.6%) as compared with the control group (40.8%). Otherwise, there were no statistically significant differences in the prevalence of comorbidities or mean laboratory values between groups."
A relatively new technology, carotid vessel wall imaging was performed on all participants on a 3-tesla magnetic resonance imaging scanner with a 16-channel head-neck-spine coil. Information collected included:
- Presence of plaque in the carotid arteries
- Presence of IPH (with laterality relative to RAO)
- Degree of carotid stenosis
A single carotid artery was selected from control patients for use in comparing the presence of IPH and the mean degree of stenosis between controls and the RAO group.
Study findings
Of the patients with RAO, five (35.7%) had imaging evidence of ipsilateral IPH. Seven of 211 (3.3%) patients in the control group had evidence of ipsilateral IPH.
Of the five patients with RAO and ipsilateral IPH, only one (20.0%) was found to have ipsilateral carotid stenosis greater than 70%. Carotid IPH was the only variable that was independently associated with RAO (odds ratio 12.6, 95% confidence interval = 2.2-73.6, P = 0.005).
The mean degree of ipsilateral carotid stenosis in all patients with RAO was 26.7% ± 29.9%, compared with 8.8% ± 22.4% in randomly selected carotid arteries in control patients (P = 0.005).
In arteries with IPH, there was no difference in the mean degree of carotid artery stenosis between the RAO and the control groups (44.8% ± 29.5% versus 55.0% ± 32.1%, P = 0.51).
One patient of five with IPH (20.0%) in the RAO group was found to have ipsilateral carotid artery stenosis greater than 70% compared with three of seven patients (42.9%) with IPH in the control group.
"Our study has three primary findings," says Dr. Bhatti. "First, we found that patients with RAO had a statistically significant higher prevalence of IPH (as seen on HR-MRA carotid plaque imaging within six weeks of the event) as compared with asymptomatic control subjects. Second, the presence of IPH was independently associated with ipsilateral RAO. And third, we observed that a low percentage (20%) of patients with RAO were found to have IPH in the setting of greater than 70% carotid stenosis.
"These findings support the use of plaque imaging in the diagnostic evaluation of patients with acute retinal ischemic events and emphasize that detecting and managing carotid artery disease is not just based on the traditional thinking that more than 70% stenosis is clinically significant and requires surgical intervention."
For more information
Larson AS, et al. The frequency of carotid intraplaque hemorrhage on vessel wall imaging in patients with retinal artery occlusion: A cross-sectional prevalence study. Journal of Neuro-Ophthalmology. In press.