July 27, 2022
Retinopathy in right eye
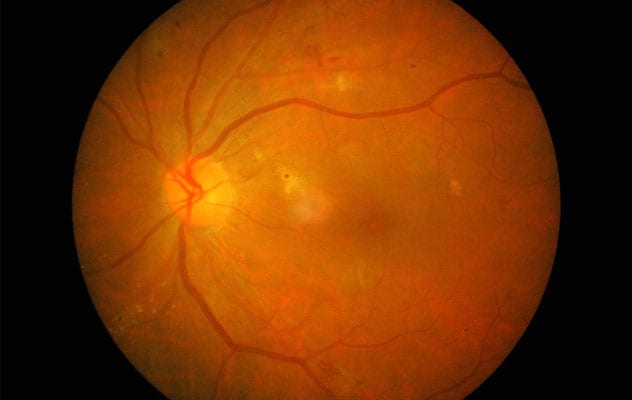
Retinopathy in right eye
Retinal image of right eye in uncontrolled type 2 diabetes with decreased visual acuity and hyperglycemia.
A retrospective study of a population-based cohort of children (younger than 22 years) diagnosed with diabetes during a 50-year period found that those with type 2 diabetes (T2D) developed vision-threatening retinopathy after a shorter diabetes duration and at a higher rate than did children with type 1 diabetes (T1D).
"Despite the increasing prevalence of T2D diagnosed in childhood, little is known about the natural history of ocular sequelae in youth-onset T2D compared with T1D," says Brian G. Mohney, M.D., an ophthalmologist, at Mayo Clinic in Rochester, Minnesota. "Current pediatric diabetic retinopathy screening follows evidence-based guidelines for children diagnosed with T1D, but data guiding the management of diabetic retinopathy in childhood-onset T2D are limited."
To assess the risk of children developing diabetes-associated ocular complications, Dr. Mohney and fellow researchers used Rochester Epidemiology Project data to conduct a retrospective, population-based medical record review of all residents of Olmsted County, Minnesota, diagnosed with diabetes at ages younger than 22 years between 1970 and 2019.
The research team confirmed a diagnosis of T1D for inclusion if the medical record reported a diagnosis of insulin-dependent diabetes mellitus, or T1D, with subsequent treatment consistent with management of T1D. A diagnosis of T2D was confirmed as noninsulin-dependent diabetes mellitus, or T2D. Among 1,362 individuals with a diagnostic code of diabetes before 22 years of age, 606 met inclusion criteria.
Diabetes-associated ocular complications assessed in the study included nonproliferative diabetic retinopathy, proliferative diabetic retinopathy, diabetic macular edema, a visually significant cataract, and the need for pars plana vitrectomy.
Cohort characteristics
During the 50-year period, 606 children were diagnosed with diabetes, yielding an incidence of T1D of 26 per 100,000 children per year and an incidence of T2D of 5 per 100,000 per year. Of the 606 children diagnosed, 525 underwent at least one eye examination and sufficiently met diagnostic criteria to distinguish between T1D (461 participants) and T2D (64 participants). Cohort characteristics included:
- The mean age at diabetes diagnosis was 12.1 years.
- Of the 525 participants, 261 were female and 264 were male.
- White children (384 participants) constituted a significantly larger percentage of the T1D cohort compared with the T2D cohort (35 participants). There were 9 children of Asian descent with T1D and 3 with T2D and 12 Black children with T1D and 21 with T2D.
- The proportion of female participants in the T2D cohort was significantly higher than that in the T1D cohort.
- Those patients with T2D were more likely to have a blood pressure of greater than 130/80 mm Hg or be using antihypertensive medications at the initial diagnosis of diabetic retinopathy compared with patients with T1D.
- Diabetes-associated ocular complications occurred in 147 of the 461 children with T1D and in 17 of the 64 children with T2D.
The hazard ratios illustrating the risk between T2D and T1D rates of developing complications were:
- 1.88 for any diabetic retinopathy (nonproliferative or proliferative diabetic retinopathy)
- 2.33 for proliferative diabetic retinopathy
- 1.49 for diabetic macular edema
- 2.43 for a visually significant cataract
- 4.06 for requiring pars plana vitrectomy by 15 years after the diagnosis of diabetes
The prevalence of diabetic retinopathy, including both nonproliferative diabetic retinopathy and proliferative diabetic retinopathy, was 32.6% at 15 years after diagnosis among all patients with documentation of eye examinations during a mean follow-up of 13 years, with 18 individuals dying before 40 years of age.
"In this study, children diagnosed with T2D had a higher risk of developing diabetic retinopathy, developing proliferative diabetic retinopathy, and requiring pars plana vitrectomy compared with those diagnosed with T1D," notes Dr. Mohney. "The duration between the diagnosis of diabetes and the development of diabetic retinopathy was shorter in the T2D cohort compared with the T1D cohort, and patients with T2D developed vision-threatening retinopathy at a higher rate than those with T1D."
"This data suggests that the natural history of retinopathy development among youth diagnosed with T2D may differ from that in youth diagnosed with T1D — that patients with T2D may be more susceptible to developing retinopathy than those with T1D despite controlling for diabetes disease duration. Children with T2D may require ophthalmoscopic evaluations at least as frequently as or more frequently than children with T1D to prevent serious ocular complications."
For more information
Rochester Epidemiology Project.
Bai P, et al. Ocular sequelae in a population-based cohort of youth diagnosed with diabetes during a 50-year period. JAMA Ophthalmology. 2022;140:51.
Refer a patient to Mayo Clinic.