June 19, 2021
Mayo Clinic has demonstrated that in utero repair of myelomeningocele can improve hindbrain herniation prenatally. As a result, complications associated with myelomeningocele at birth, such as Chiari malformation and hydrocephalus, can often be avoided.
"We're finding that about 90% of the prenatal myelomeningocele repairs that we perform result in reversal of brain malformation before birth. This is a big breakthrough for children with spina bifida," says Edward S. Ahn, M.D., a neurosurgeon at Mayo Clinic Children's Center in Rochester, Minnesota.
Prenatal myelomeningocele repair is performed by a multidisciplinary team led by Dr. Ahn and a Maternal and Fetal Medicine specialist. The team also includes pediatric and adult anesthesiologists, pediatric cardiologists to continuously monitor fetal cardiography, and specialized nursing support. All patients have ultrasound and MRI performed by neuroradiologists with specialized training.
"Without surgical intervention, the natural course for these babies is a severe congenital spinal defect that can cause motor weakness and bladder problems," Dr. Ahn says.
Cerebrospinal fluid that leaks through the meningocele can cause Chiari malformation, which in turn can lead to hydrocephalus requiring ventriculoperitoneal shunt placement after birth. Prenatal repair also prevents the spinal cord's exposure to amniotic fluid, which may be toxic to the spinal cord.
Myelomeningocele is generally diagnosed through routine fetal ultrasound during the second trimester of pregnancy. Surgical repair can be performed between 19 and 26 weeks of gestation. When possible, Mayo Clinic specialists prefer to perform surgery at around 24 or 25 weeks of gestation, when the fetus is slightly larger.
In addition to their expertise with open surgical repair, Mayo Clinic surgeons have experience performing myelomeningocele repair fetoscopically. That minimally invasive approach lessens the risk of preterm birth and allows the mother to have a vaginal delivery during that pregnancy and in subsequent pregnancies.
Elucidating prenatal benefits
In utero myelomeningocele repair
In utero myelomeningocele repair
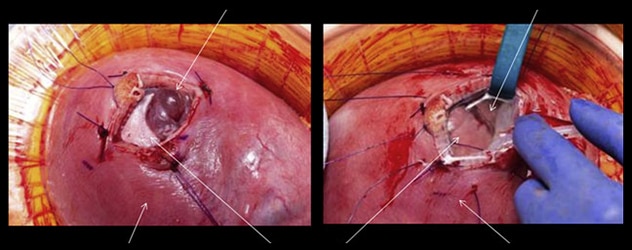
Photographs show in utero open repair of fetal myelomeningocele at 25 weeks of gestation. On the left, myelomeningocele is apparent (top white arrow). On the right, the spinal defect has been closed (top white arrow).
Using MRI, Mayo Clinic researchers have documented improvement in hindbrain herniation as soon as six weeks after prenatal myelomeningocele repair. A study published in the April 2020 issue of Mayo Clinic Proceedings reports three consecutive fetuses with prenatally diagnosed myelomeningocele that had in utero repair between 24 and 25 weeks of gestation. All three fetuses had lumbosacral defects with evidence of hindbrain herniation.
MRI performed six weeks after prenatal open surgical repair showed improvement in hindbrain herniation in all three fetuses. Deliveries occurred at 37 weeks' gestation via cesarean section without notable complications. Postnatal follow-up examinations were generally unremarkable, with one baby having mild ventriculomegaly at 3 months of age.
"We would expect to see the same degree of improvement when myelomeningocele repair is performed fetoscopically," Dr. Ahn says.
In utero myelomeningocele repair is part of Mayo Clinic's broader prenatal regenerative therapy program. Through that program, Mayo Clinic seeks to provide specific fetal interventions with the potential to promote regrowth and redevelopment of malformed organs. "The idea is to restore normal development before birth," Dr. Ahn says.
As a multispecialty center, Mayo Clinic has expertise in both maternal and fetal care. "We have specialists taking care of the mother and the fetus, and then the neonate, all under one roof. Maternal and Fetal Medicine specialists are involved from the very beginning," Dr. Ahn says. "We convene regularly to review our procedures and to innovate and improve those procedures."
In addition, the spinal bifida clinic on the Rochester campus of Mayo Clinic coordinates care for children and teenagers with the condition.
"It's a privilege for us at Mayo Clinic to care for these children from before they're born to the time they're growing up and reaping the benefits of this prenatal intervention," Dr. Ahn says.
For more information
Ruano R, et al. In utero restoration of hindbrain herniation in fetal myelomeningocele as part of prenatal regenerative therapy program at Mayo Clinic. Mayo Clinic Proceedings. 2020;95:738.