Oct. 01, 2022
Mayo Clinic's Pediatric Brain Tumor Clinic uses cutting-edge neuroimaging and 3D anatomic models to inform optimal treatment and aid with surgical planning. Mayo Clinic is a pioneer in these areas, having developed unique neuroimaging modalities and the largest point-of-care manufacturing facility for 3D-printed, life-size, patient-specific models in the United States.
"Pediatric brain tumors require expertise at every step of the way. Our neuroradiologists, neurosurgeons, neuropathologists, radiation oncologists and neuro-oncologists have the skill and technology to care for these kids in the best multidisciplinary way," says Jonathan M. Morris, M.D., a neuroradiologist at Mayo Clinic in Rochester, Minnesota.
Part of Mayo Clinic Children's Center, the Pediatric Brain Tumor Clinic uses functional MRI to map speech, motor and sensory pathways before surgery. Advanced intraoperative monitoring, including sensory cortex neuromonitoring and intraoperative MRI, is also routinely used.
"Intraoperative MRI allows us to be very specific in our tumor resection," says David J. Daniels, M.D., Ph.D., a pediatric neurosurgeon at Mayo Clinic's campus in Minnesota. "If any residual tumor is seen on intraoperative MRI, we can resect it right away rather than waiting to get an MRI and going back into surgery the next day."
Mayo Clinic is one of the few centers in the United States with clinical 7-tesla MRI, which provides a magnetic field more than twice as strong as that of conventional 3-tesla MRI. The extra field strength greatly improves clarity, contrast and resolution when imaging brain tumors in children. 7-tesla MRI can be used for children who weigh at least 75 pounds (34 kilograms).
Magnetic resonance elastography — invented and available only at Mayo Clinic — assesses the firmness of a tumor compared with healthy brain tissue to help plan safe surgical procedures. Slip interface imaging, also developed at Mayo Clinic, reveals the extent of tumor adhesion to healthy brain tissue.
"Slip interface imaging allows us to see how the waves pass between normal brain and tumor tissue and to determine whether the tissues are adherent at that interface," says John Huston, III, M.D., a neuroradiologist at Mayo Clinic's campus in Minnesota. "We're now providing information that previously wasn't really possible to get preoperatively."
Patient-specific 3D-printed models
Tumor MRI
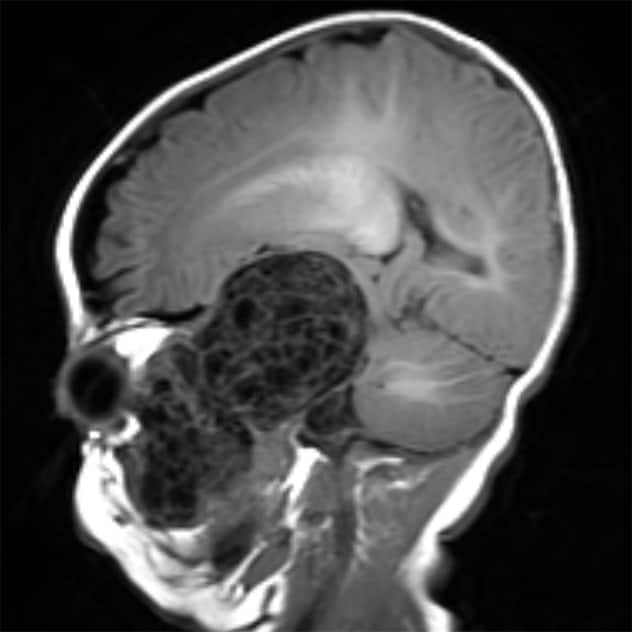
Tumor MRI
Sagittal MRI shows a brain tumor extending into the face of a 1-year-old child.
3D reconstruction
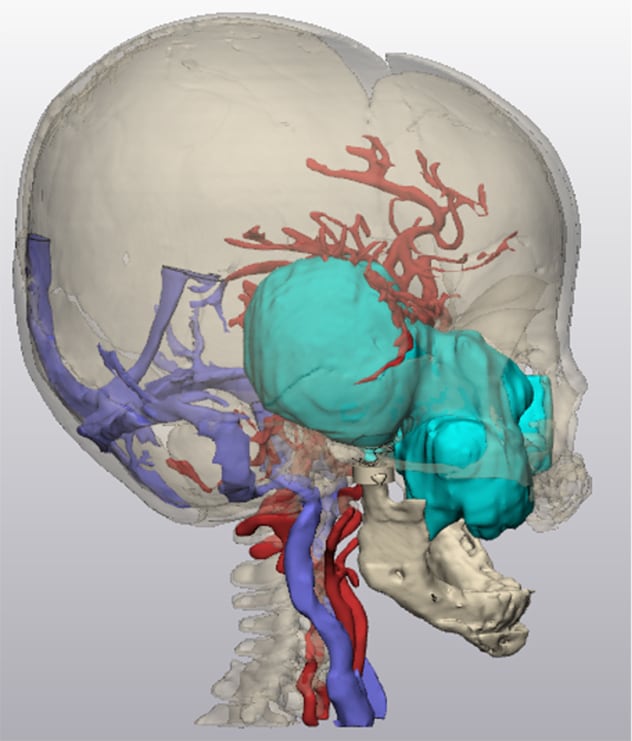
3D reconstruction
Image shows a 3D reconstruction of the child's tumor based on imaging data.
3D-printed model
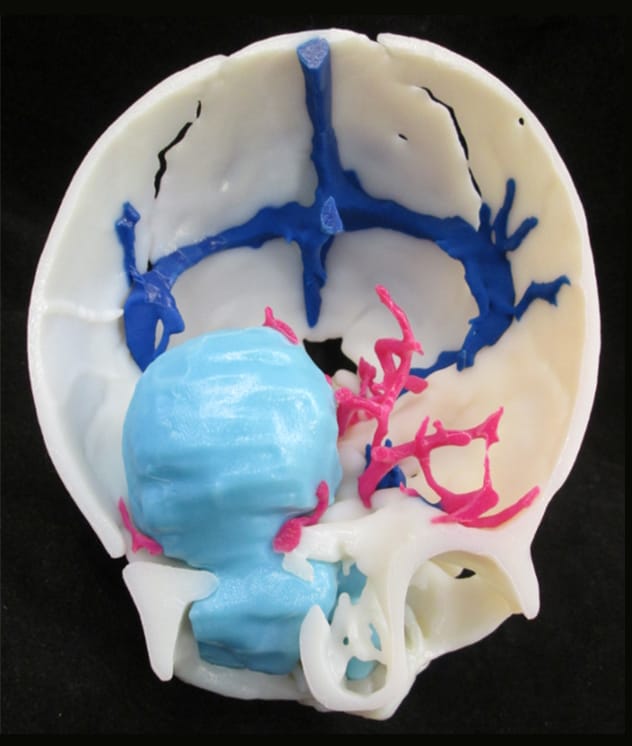
3D-printed model
Photograph shows a 3D-printed model created at Mayo Clinic to optimize the child's treatment.
State-of-the-art 3D printing facilitates patient and family education as well as the planning of surgical and radiation procedures.
"We're able to give our neurosurgeons a life-sized, patient-specific model of a child's brain, tumor, skull and surrounding vasculature," says Dr. Morris, who serves as medical director of Mayo Clinic's 3D Anatomic Modeling Laboratories. "Our surgeons don't have to rely on their ability to create 3D pictures based on thousands of images from CT and MRI scans. They can hold a patient-specific model in their hands, which allows for haptic perceptions."
The models are especially helpful for surgery involving complex tumors. "When tumors are located in or around important structures — such as the cranial nerves, brainstem or cerebrovascular vessels — it's advantageous to see those relationships in 3D before going to surgery," Dr. Daniels says.
The anatomic modeling unit is located within the Department of Radiology, facilitating interaction among neuroradiologists, neurosurgeons and clinical engineers. "We can move rapidly from customized CT and MRI protocols to the creation of 3D images to the manufacturing of patient-specific, 3D-printed models," Dr. Morris says.
The manufacturing process starts with CT and volumetric MRI of a patient, using imaging protocols designed by Mayo Clinic radiologists specifically for 3D printing. A Mayo Clinic radiologist evaluates the accuracy of the imaging data before the model is produced.
"Our patient-specific models aren't developed solely by algorithms or employees who may not fully understand neuroanatomy and neuropathology," Dr. Morris says. "The biomedical engineers in our facility are part of the clinical care team, routinely working with radiologists and surgeons on a daily basis. The life-sized model we give to the surgeon is exactly what the surgeon is going to find during the patient's procedure."
Virtual reality
Once the 3D model is created, it can be used in formats other than anatomic modeling and 3D printing. The 3D data can be loaded onto phones or tablets and manipulated on-screen or placed into virtual or augmented reality.
Mayo Clinic plans to offer presurgical virtual reality experiences when appropriate. "We can take a child, if old enough, and parents with the surgeon into virtual reality together, to allow them to see the brain tumor in a way they wouldn't otherwise," Dr. Morris says.
Mayo Clinic's commitment to these technologies highlights the importance of neuroradiologists and extended reality technologies on the pediatric brain tumor care team.
"Neuroradiology touches every child who needs brain tumor care," Dr. Morris says. "Our neuroradiologists provide essential information for planning surgery and also follow-up imaging for tumor recurrence. We have the resources to provide the best care for kids."
For more information
Pediatric Brain Tumor Clinic. Mayo Clinic.
Children's Center. Mayo Clinic.
3D Anatomic Modeling Laboratories. Mayo Clinic.
Refer a patient to Mayo Clinic.