March 20, 2021
Although retinoblastoma is the most common malignant eye tumor in children, it is a very rare cancer. State-of-the-art imaging performed by experienced pediatric neuroradiologists is the key to maximizing patient outcomes.
"Our goal is preservation of the child's life, eye and sight. That requires a multidisciplinary and highly specialized approach to accurately stage the cancer," says Victoria (Michelle) M. Silvera, M.D., chief pediatric neuroradiologist at Mayo Clinic in Rochester, Minnesota.
If the tumor is contained within the globe of the eye, eye-preserving therapy is often an option. A tumor that stretches back along the optic nerve generally requires enucleation. Rarely, retinoblastoma spreads to the intracranial space.
"So much hinges on whether the tumor is in the optic nerve. Highly detailed imaging is critical for appropriate diagnostic staging and for survival," says Julie B. Guerin, M.D., a pediatric neuroradiologist at Mayo Clinic's campus in Rochester, Minnesota. "Both high-resolution and contrast-enhanced MRI are important for identifying key features that impact treatment decisions."
At Mayo Clinic, treatment is individualized for each patient. "The treatment can be complex. It is critical to have a multidisciplinary team well versed in retinoblastoma care," says Lauren A. Dalvin, M.D., an ocular oncologist at Mayo Clinic's campus in Rochester, Minnesota, who leads the retinoblastoma care team.
Interventional neuroradiology also plays a key role. For patients with advanced disease in one eye, Mayo Clinic routinely uses intra-arterial rather than intravenous chemotherapy. "Intra-arterial chemotherapy delivers a very high dose directly to the tumor, which increases the efficacy of therapy while also minimizing side effects," says Waleed Brinjikji, M.D., a neurointerventionalist at the Rochester campus of Mayo Clinic. "There is a pretty steep learning curve with this procedure, so it's very important to have an interventional neuroradiologist with experience in treating young children."
Multidisciplinary diagnosis and treatment
Retinoblastoma treatment
Retinoblastoma treatment
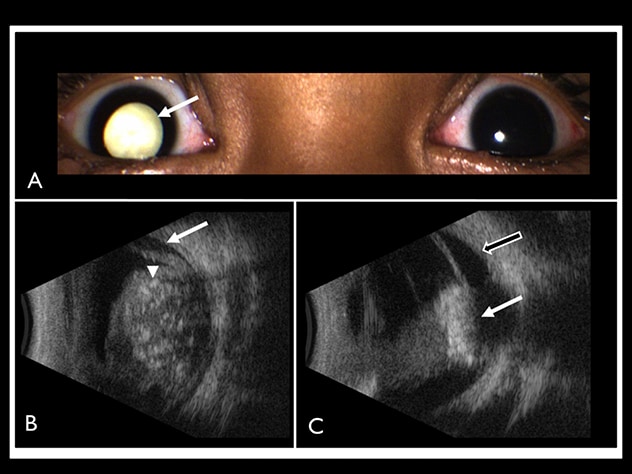
Images illustrate the treatment of a 2-year-old child with Group E retinoblastoma at Mayo Clinic. A. Photograph shows leukocoria (white arrow) in the child's right eye. B. Ultrasonography shows a large, round, hyperechoic retinal mass within the right globe, with tumor calcifications seen as foci of high reflectivity (white arrowhead) with posterior acoustic shadowing and serous detachment of the retina (white arrow). C. Following three cycles of intra-arterial and intravitreal chemotherapy, the follow-up ultrasound image shows shrinkage of the tumor to a calcified hyperechoic scar (white arrow). Minor serous retinal detachment persisted (black-and-white arrow). Images reprinted with permission from American Journal of Radiology.
Hereditary retinoblastoma
Hereditary retinoblastoma
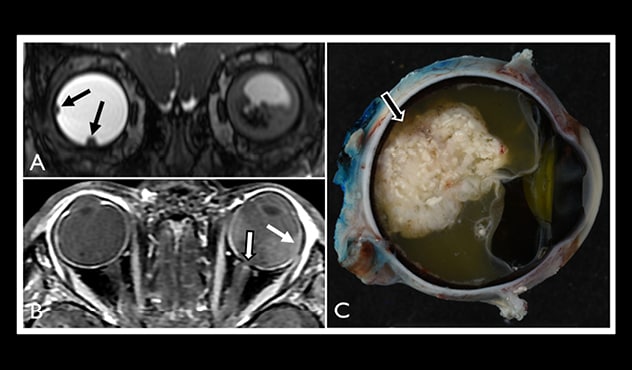
Images illustrate the treatment of a 21-month-old child with hereditary retinoblastoma, with Group B retinoblastoma of the right eye and Group E retinoblastoma of the left eye. A. Coronal 3D fast imaging employing steady-state acquisition (FIESTA) shows two small retinoblastoma tumors (black arrows) in the right globe. A hypointense mass with serous retinal detachment is visible in the left globe. B. T1-weighted post-gadolinium image with fat saturation shows interruption of the normally enhancing chorioretinal interface (white arrow), which could represent subtle choroidal invasion. MRI does not show tumor extending into the left optic nerve (black-and-white arrow). Tiny foci of enhancement surround the left optic nerve cuff, representing normal small vessels. The left globe was larger than the right, consistent with buphthalmos. Enucleation of the left eye was performed due to the buphthalmos and persistent eye redness and discomfort. C. Gross pathology specimen of the enucleated left eye demonstrated the large retinoblastoma posteriorly within the globe (arrow). Histopathology (not shown) demonstrated a moderately differentiated retinoblastoma with tumor involving the optic nerve head and no post-laminar tumor extension, as accurately diagnosed on the preoperative MRI. Images reprinted with permission from American Journal of Radiology.
Typically, retinoblastoma is first noticed by a parent or pediatrician who sees "white pupil" (leukocoria) in a child's eye. "That reflection of light, which normally passes through to the retina, is very concerning for tumor," Dr. Silvera says.
An ophthalmologist generally makes the initial diagnosis of retinoblastoma, which can be heritable or sporadic. Diagnosis of the heritable type typically occurs before age 1 and diagnosis of the sporadic type by age 2. Tumor size can range from very small to large enough to engulf the entire eye, although in the United States the disease is generally found before then.
Mayo Clinic's ophthalmological exam includes color fundus photography, ultrasonography, fluorescein angiography and optical coherence tomography. To confirm an initial diagnosis and to stage the tumor, Mayo Clinic's pediatric neuroradiologists obtain detailed images using 3-tesla MRI with a high-performance multichannel head coil.
A pediatric anesthesiologist administers general anesthesia before the imaging procedure. "Any motion by the child would degrade the image," Dr. Silvera says. "Achieving the highest-quality imaging possible is essential to identifying tumor, particularly within the optic nerve, and sparing the child a second round of general anesthesia and imaging."
Detailed imaging is necessary to check for intracranial disease, which has a poor prognosis. "The contralateral eye is also carefully assessed on imaging, particularly in children with heritable retinoblastoma," Dr. Silvera says. "Great care is needed because any contralateral tumor is typically much smaller than the tumor in the eye that presents with symptoms."
If eye-sparing treatment is an option, Mayo Clinic's ocular oncologists can administer intravitreal chemotherapy, laser therapy, cryotherapy or thermal therapy with the patient under general anesthesia. If intra-arterial chemotherapy is required, it can be administered directly afterward, while the patient is still under the same anesthesia.
The intra-arterial procedure involves threading a catheter from the femoral artery up to the ophthalmic artery. "The vast majority of these patients are under the age of 3 years, so their blood vessels are very small and fragile. It's critical to have an interventional neuroradiologist who can safely perform procedures on these very delicate children," Dr. Brinjikji says. At Mayo Clinic, patients are generally able to return home on the day of the procedure.
Brachytherapy is another treatment option for retinoblastoma that does not respond well to chemotherapy. To prevent side effects, Mayo Clinic generally avoids external beam radiotherapy for children with retinoblastoma.
Patients who require enucleation can have the procedure at Mayo Clinic and then be fitted with a prosthesis. "The prostheses nowadays are very good and natural appearing," Dr. Silvera says.
Follow-up imaging is another important aspect of care. "We're looking for recurrence of tumor in the affected orbit but also in the contralateral globe if the child has the genetic form of retinoblastoma, and for tumor in the brain," Dr. Silvera says.
Children with retinoblastoma are at risk of developing retinoblastoma-like tumor in deep portions of the brain, specifically in the pineal and parasellar regions. Recurrent tumor in these regions is called trilateral or quadrilateral retinoblastoma, depending on the extent of tumor. "We look carefully for this on follow-up MRI, as this type of recurrence needs to be managed promptly. It carries a poor prognosis," Dr. Guerin says.
Initially, most patients are seen once a month, with appointments often coordinated with cycles of chemotherapy. Over time, if the cancer has completely regressed, the time between visits might be slowly extended. "Most recurrences happen within the first three years, so we keep close tabs on these children during that period," Dr. Dalvin says. "After that, the interval between visits might be extended to six to 12 months."
In developed countries, the survival rate for retinoblastoma is over 98%. Globe salvage rates have improved with the introduction of intra-arterial chemotherapy. For children with Group E disease — the most advanced stage — salvage rates are about 50%. "For Group D eyes, we can save nearly 80%," Dr. Dalvin says. "The globe salvage for less advanced Groups A, B and C is over 90%."
Mayo Clinic organizes retinoblastoma care to make it as efficient and effective as possible for the child and the family. "Retinoblastoma is a complex disease," Dr. Silvera says. "It requires an expert, multidisciplinary team and a long-term commitment to the patient and family."
For more information
Silvera VM, et al. Retinoblastoma: What the neuroradiologist needs to know. American Journal of Neuroradiology. January 2021.