Oct. 02, 2020
Mayo Clinic is conducting a major study aimed at identifying mechanisms and predictors of persistent post-traumatic headache attributed to mild traumatic brain injury. With funding from the Department of Defense, the study includes a phase II clinical trial of erenumab for treatment of this type of headache.
"We have a long way to go in truly understanding why two people can have very similar brain injuries, yet one person gets persistent and disabling post-traumatic headache and the other does not," says Todd J. Schwedt, M.D., a neurologist at Mayo Clinic in Phoenix/Scottsdale, Arizona. "With this large, multifaceted research program, we are trying to find predictors, as well as ways of intervening, so these headaches don't persist."
Although post-concussion symptoms often resolve within a few days, persistent symptoms, including headache, can be a debilitating consequence of mild traumatic brain injury. Up to 40% of individuals who develop acute post-traumatic headache will experience persistent headache, defined as continuing for more than three months after injury.
"Persistent post-traumatic headache can be quite disabling," Dr. Schwedt says. "A lot of patients have continuous headache pain with superimposed exacerbations. Many have symptoms resembling migraine, such as light sensitivity, sound sensitivity, nausea, and worsening of symptoms with routine physical and mental activities."
Mayo Clinic's study includes investigations of animal models of post-traumatic headache as well as human studies of potential blood biomarkers, structural and functional brain imaging, and neurophysiological testing. "We will investigate how a person with post-traumatic headache processes visual and painful stimuli, giving us insights into post-traumatic headache pathophysiology," Dr. Schwedt says.
Participants in the clinical trial portion of the study will be randomized to receive a placebo or erenumab, a calcitonin gene-related peptide (CGRP) receptor monoclonal antibody. That randomization will occur when a participant has experienced post-traumatic headache for 35 to 56 days.
Dr. Schwedt notes that optimal timing for therapeutic intervention will need further study. "The outcomes might be different, depending on when intervention occurs," he says. "There are several potential time points for intervention — an acute period within the first few days of a head injury, a subacute period of a few days to a couple of months after injury, and a chronic period when headaches have already been present for several months. Clinical trials are needed that include therapeutic interventions during each of these time points."
Elucidating headache subtypes
Mayo Clinic is at the forefront of efforts to stratify patients' risk of post-traumatic headache and to find targeted therapies. Directed by Dr. Schwedt, the Neuroimaging of Headache Disorders Laboratory has identified aberrations in brain structure and function that are related to post-traumatic headache due to concussion.
"Although brain-imaging studies after concussion are typically considered normal when they are performed for clinical reasons, when we look more closely in our research studies, we often find subtle abnormalities in brain structure and function," Dr. Schwedt says.
Many of the laboratory's studies compare symptoms of post-traumatic headache and migraine, as well as brain structure and function in the two headache types. "There is a lot of overlap in symptoms between persistent post-traumatic headache and migraine," Dr. Schwedt says. "On imaging, we see what we consider to be meaningful differences both in brain structure and functional connectivity. Although there may be some shared pathophysiology in the two headache types, we believe there is also distinct pathophysiology for post-traumatic headache."
Structural differences in brain regions comparing persistent post-traumatic headache migraine
Structural differences in brain regions comparing persistent post-traumatic headache migraine
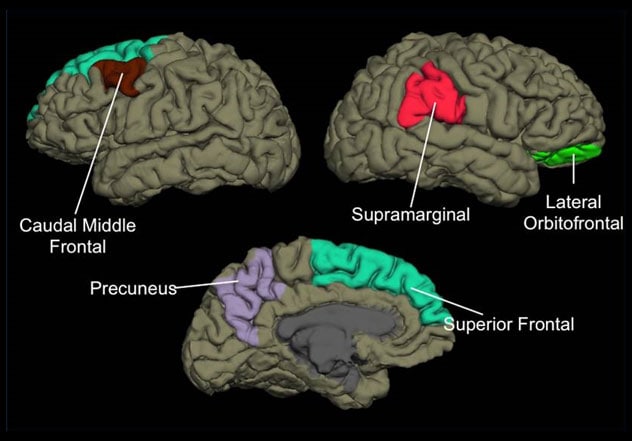
Illustration shows the brain regions with structural differences when individuals with persistent post-traumatic headache are compared with individuals with migraine. Illustration reprinted with permission from The Journal of Headache and Pain.
In research published in The Journal of Headache and Pain in 2017, Mayo Clinic shared results of a study comparing brain structures in individuals with persistent post-traumatic headache to the brain structures of individuals with migraine. Results showed that the right lateral orbitolfrontal region differed in area, volume and curvature. The left caudal middle frontal, precuneus and gyrus regions differed in in cortical thickness.
Mayo Clinic is committed to continuing studies of the likely multifactorial pathophysiology of post-traumatic headache. "Our ongoing investigations will ultimately improve our ability to treat patients with this disabling condition and improve our ability to prognosticate outcomes for individuals with post-traumatic headache," Dr. Schwedt says.
For more information
Neuroimaging of Headache Disorders Laboratory: Todd J. Schwedt. Mayo Clinic.
Schwedt TJ, et al. Persistent post-traumatic headache vs. migraine: An MRI study demonstrating differences in brain structure. The Journal of Headache and Pain. 2017;18:87.