Aug. 20, 2021
Mayo Clinic stresses multidisciplinary and patient-centered management of pituitary tumors, generally resulting in fewer surgical complications and shorter hospital stays. Approximately 82% of patients are sent home the day after surgery.
The type of surgery performed is tailored to an individual's needs. "No single person controls our pituitary tumor practice. Our multidisciplinary team ensures that many eyes and ears are going over each patient, from pre-surgical to post-surgical care," says Jamie J. Van Gompel, M.D., a neurosurgeon at Mayo Clinic in Rochester, Minnesota.
Mayo Clinic has neurosurgeons with expertise in both microsurgical and endoscopic pituitary tumor resections. Nationwide, the endoscopic approach is increasingly favored — although its impact on improving patient care hasn't been elucidated. A retrospective study comparing 534 microsurgical and endoscopic pituitary tumor surgeries at Mayo Clinic between 2014 and 2019 documented a similar number of patients having each procedure.
The study, published in the August 2021 issue of Mayo Clinic Proceedings, set out to document the advantages and disadvantages of the microscopic and endoscopic approaches performed at a single center. Among the patients studied, one neurosurgeon performed all microscopic resections and a second neurosurgeon performed all endoscopic procedures.
The study demonstrated that both approaches are safe and can substantially benefit patients. "In experienced hands at an experienced center, the overall outcome of pituitary tumor surgery is excellent, whether the procedure is done with a microscope or an endoscope," Dr. Van Gompel says.
The study also found differences between Mayo Clinic's outcomes and those reported in a multicenter study published in the April 2020 issue of the Journal of Neurosurgery:
- 3.4% of Mayo's patients were readmitted to the hospital within 30 days of surgery compared with 9.5% of patients treated microscopically and 6.3% treated endoscopically in the multicenter study.
- Hospital stays averaged 1.3 days at Mayo Clinic compared with three days reported in the multicenter study.
- Mayo Clinic had significantly shorter operating times, with microsurgery averaging 83 minutes and endoscopic procedures averaging 131 minutes — compared with 219 minutes for microsurgery and 293 minutes for endoscopic procedures in the multicenter study.
"Our patients did very well, with few secondary treatments," Dr. Van Gompel says. "Pituitary tumors were commonly taken care of with one operation."
Expertise in endocrinology and neuroradiology
Mayo Clinic is committed to multispecialty management of pituitary tumors. Neurosurgeons, endocrinologists and neuroradiologists have interdisciplinary conferences to determine the correct diagnosis and optimal treatment in challenging cases.
The endocrinologists — part of Mayo Clinic's Pituitary-Gonad-Adrenal (PGA) Specialty Group — are typically the first physicians to see patients with pituitary tumors.
"Our wealth of experience allows us to provide state-of-the-art care to patients with all types of pituitary tumors," says Dana Erickson, M.D., an endocrinologist at Mayo Clinic in Minnesota. "We provide a comprehensive clinical assessment that focuses on the patient as a whole, including evaluation of comorbidities associated with functional tumors or hypopituitarism."
Dynamic pituitary testing is performed in Mayo Clinic's Endocrine Testing Center. In the setting of Cushing syndrome, endocrinologists work closely with neurosurgeons and neuroradiologists to organize inferior petrosal sinus sampling and 7-tesla MRI.
"We have made great strides with our clinical 7-tesla imaging," says Jason T. Little, M.D., a neuroradiologist at Mayo Clinic in Minnesota. "A known drawback of scanning at 7-tesla is the characteristic artifact from the skull base, which can obscure the pituitary gland. But working with our MRI physicists, we have been able to mitigate that artifact with our 7-tesla scanner."
Mayo Clinic also uses 3-tesla MRI with dynamic contrast as needed. "That allows us to detect subtle but clinically important small pituitary tumors," Dr. Little says.
Microscopic versus endoscopic pituitary surgery
Microscopic versus endoscopic pituitary surgery
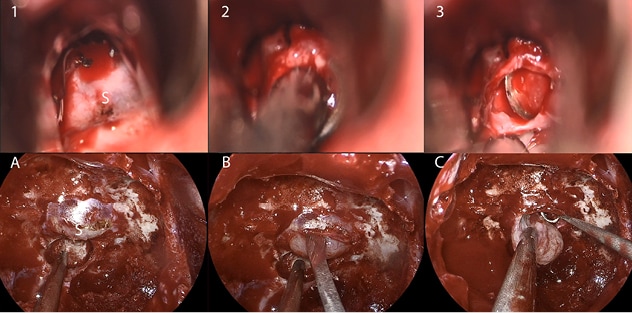
Photographs taken during a microscopic pituitary surgery (top) and an endoscopic pituitary surgery (bottom) show the surgical exposures in patients with similar midline macroadenomas. 1. Photograph shows the view with the microscope through a speculum to the face of the sella. 2. The surgeon brings the tumor midline through the dural opening to suction for resection. 3. The surgeon uses a curet to look through the microscope to assess the gland after the tumor's removal. A. The view of the sella in the endoscopic procedure is comparable to the microscopic exposure seen in 1. B. The surgeon dissects the gland upward off the tumor with a dissector rather than using intratumoral resection, as was used in the microscopic procedure. C. The extracapsular bimanual resection of the pituitary tumor off the gland continues, with a suction and curet similar in size to the curet seen in 2. Image reprinted with permission from Mayo Clinic Proceedings.
The multidisciplinary team recommends surgery, medical treatment or active surveillance. If surgery is needed, the microscopic and endoscopic approaches offer differing views of pituitary tumors.
Mayo Clinic's study confirmed that the endoscopic approach generally provides a larger percentage of tumor resection. Nevertheless, both approaches achieved a high volume of tumor resection: 87% for microscopic procedures and 92% for endoscopic procedures.
"Our group has previously published that 85% resection is commonly needed to avoid secondary therapy, and we exceeded that level with both approaches," Dr. Van Gompel says. "Larger or more-invasive tumors probably benefit from an endoscopic approach. But for tumors that are likely to measure less than 2 centimeters and are confined to the pituitary gland, the technique doesn't matter much."
Post-surgical complications among patients in the study were generally low:
- 0.4% of patients developed post-surgical infections.
- Approximately 2% of patients had post-surgical cerebral spinal fluid leaks compared with 4.9% of patients treated microscopically and 3.4% treated endoscopically in the multicenter study.
- 8% of Mayo Clinic patients had new anterior pituitary dysfunction, and 2.8% had permanent posterior dysfunction.
Mayo Clinic provides extensive follow-up care for patients who have pituitary tumor surgery. A nurse specializing in pituitary care offers postoperative patient education. Other follow-up care includes imaging studies, hormone replacement therapy for hypopituitarism and adjuvant therapy if persistent disease is present in cases of functional tumors.
"Safe care can be delivered over time by a large, multidisciplinary group that specializes in pituitary practice," Dr. Van Gompel says. "Patients can benefit substantially, with low numbers of complications and a reduction in the number of treatments needed."
For more information
Van Gompel JJ, et al. Pituitary tumor surgery: Comparison of endoscopic and microscopic techniques at a single center. Mayo Clinic Proceedings. 2021;96:2043.
Little AS, et al. Results of a prospective multicenter controlled study comparing surgical outcomes of microscopic versus fully endoscopic transsphenoidal surgery for nonfunctioning pituitary adenomas: The Transsphenoidal Extent of Resection (TRANSSPHER) study. Journal of Neurosurgery. 2020;132:1043.