April 15, 2021
Mayo Clinic has reported the first case series of transvenous embolization of paraspinal veins to treat cerebral spinal fluid (CSF)-venous fistulas. The innovative therapy resulted in clinical and radiographic improvement and no permanent complications in all participants in the small case series.
"It's a significant advance in the treatment of CSF-venous fistulas," says Waleed Brinjikji, M.D., a neurointerventionalist at Mayo Clinic in Rochester, Minnesota. "We are able to fix these fistulas and send patients home the same day, without worrying about the complications that can occur with spinal surgery."
CSF-venous fistulas, first described in 2014, are increasingly recognized as a cause of spontaneous intracranial hypotension. "We are finding that, in at least a quarter of people with a CSF leak, it's due to a fistula. That is a major subgroup, and we expect it to grow as our diagnostic techniques advance," says Jeremy K. Cutsforth-Gregory, M.D., a neurologist who leads the CSF dynamics clinic at Mayo Clinic's campus in Rochester.
The most effective treatment for a CSF-venous fistula has been surgical intervention that includes laminectomy, facetectomy and ligation of the nerve root and associated veins. Although the procedure can ease the severe headaches associated with intracranial hypotension, it requires a hospital stay and lengthy recovery. Existing minimally invasive treatment options, such as epidural blood patch and fibrin glue injection, have been effective in only a tiny minority of patients with fistulas.
"Embolization seemed like a feasible alternative, as long as we could navigate through the paraspinal venous system and get our catheter to the exact right point," Dr. Brinjikji says.
Dr. Brinjikji had acquired a medical textbook from the 1970s on spinal phlebography, a common diagnostic tool before MRI. "We realized that if physicians could get into the paraspinal veins back then, we — with all the advances in catheterization — should be able to get into them and block them off using our newer and safer embolic agents," he says.
DSM to localize fistulas
Cerebral spinal fluid (CSF)-venous fistula
Cerebral spinal fluid (CSF)-venous fistula
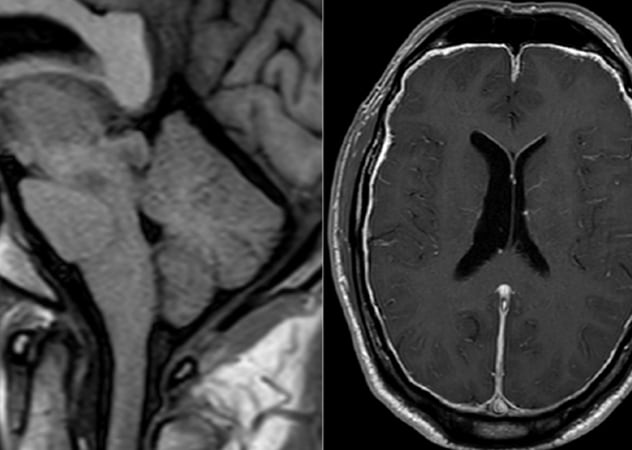
Preoperative MRI of a participant in Mayo Clinic's case series shows signs of brain sag with flattening of the pons, reduced mamillopontine distance and effacement of the suprasellar cistern, as well as thick pachymeningeal enhancement.
Embolization of CSF-venous fistula
Embolization of CSF-venous fistula
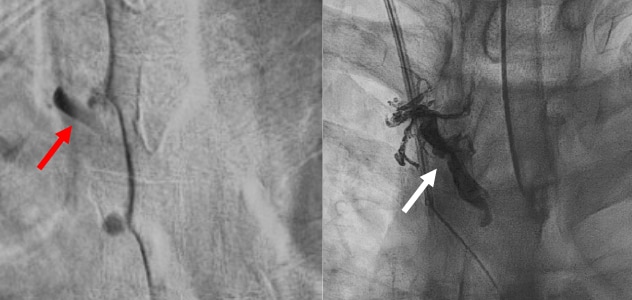
On the left, digital subtraction myelogram shows a large CSF-venous fistula at right T4 with filling of the right T4 paraspinal vein (red arrow). On the right, the patient underwent successful embolization of the vein (white arrow).
Resolution of brain sag
Resolution of brain sag
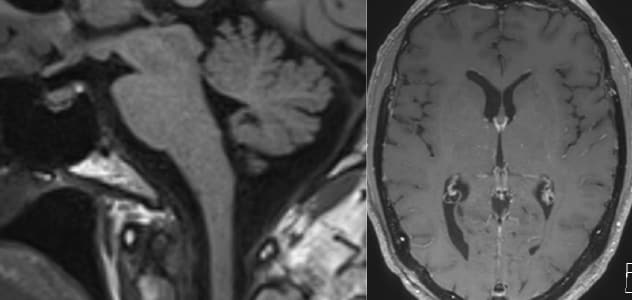
Postoperative MRI shows resolution of the brain sag and meningeal enhancement.
As described in the May 2021 issue of the American Journal of Neuroradiology, the Mayo Clinic case series included five patients with CSF hypotension secondary to CSF-venous fistulas. The patients' fistulas were localized using lateral decubitus digital subtraction myelography (DSM). On MRI, all patients had evidence of CSF hypovolemia, including brain sag and pachymeningeal enhancement with no extradural fluid collection on total spine MRI.
The endovascular procedures — performed in August 2020 — involved catheterization of the azygous vein, followed by selective catheterization and embolization of the paraspinal vein.
All patients had improved clinical and radiological findings after the procedure. Four patients had complete resolution of headaches, and one had a 50% reduction in headache symptoms. Brain sag resolved in four patients and improved but did not resolve in one patient. Similarly, pachymeningeal enhancement resolved in four patients and improved but did not resolve in one patient.
"Patient satisfaction has been very high, and we are very rigorous in obtaining complete clinical and imaging follow-up on all patients," Dr. Brinjikji says.
Pain localized to the site of the embolization was a common minor complication, but no patient required narcotics. And the pain subsided in a matter of weeks for all patients. No patient experienced permanent neurological complications. The researchers note that further studies are needed to confirm the technique and to validate the treatment's durability.
An essential component of this procedure is state-of-the-art imaging for the diagnosis of CSF-venous fistulas.
"Identifying the fistula is a major challenge," Dr. Cutsforth-Gregory says. "DSM allows us to locate fistulas that might otherwise be overlooked. It's practice changing." Currently, eight DSMs a week are routinely performed at the Rochester campus of Mayo Clinic, making it one of the highest-volume CSF leak practices in the world.
The development of innovative treatments is facilitated by Mayo Clinic's multidisciplinary approach. "Our new treatment modality results from teamwork by headache neurologists, interventional neuroradiologists and endovascular neurosurgeons, as well as a radiology team at the forefront of medical imaging," Dr. Brinjikji says. "This represents a paradigm shift — we are now using endovascular procedures to fix problems outside the vessels themselves."
For more information
Brinjikji W, et al. A novel endovascular therapy for CSF hypotension secondary to CSF-venous fistulas. American Journal of Neuroradiology. 2021;42:882.
Refer a patient to Mayo Clinic.