Jan. 11, 2019
The brachial plexus injuries experienced by newborns can range from a few stretched nerves to the tearing or rupturing of all nerves in the brachial plexus network. A multidisciplinary approach is beneficial to achieving optimal outcomes.
The brachial plexus clinic at Mayo Clinic, which manages care for children and adults, is one of the highest-volume brachial plexus clinics in the country. The treatment team includes two orthopedic hand and microsurgeons, as well as a pediatric orthopedic surgeon and a neurosurgeon specializing in peripheral nerve surgery. Subspecialized radiologists and anesthesiologists with experience in diagnostic and surgical procedures for these young patients also are available.
Appointments for patients with these injuries are generally made within a week or two of referral. Ideally, the required nerve surgery should be performed early, to avoid muscle degeneration due to the lack of nerve signals.
"We know that if you wait too long for that initial surgery — just observing for the baby's first year — you can lose the ability to do primary nerve surgery. Typically, the nerves need to be operated on in the first six months of life," says Alexander Y. Shin, M.D., an orthopedic hand and microsurgeon specializing in brachial plexus injuries at Mayo Clinic Children's Center in Rochester, Minnesota.
The benefits of an integrated approach can be seen throughout the process of managing neonatal brachial plexus injuries. Diagnosis generally involves MRI and nerve tests. At Mayo Clinic, pediatric neurologists, radiologists and anesthesiologists coordinate to perform testing in one setting.
"Otherwise, a baby might end up having two or three major anesthesia procedures. We try to minimize anesthesia to one when possible," Dr. Shin says.
Neonatal brachial plexus injury surgery
Neonatal brachial plexus injury surgery
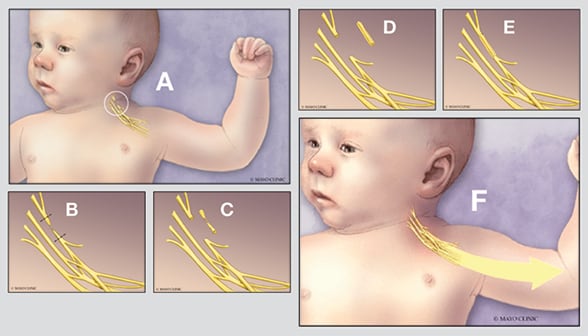
Illustration shows what occurs during neonatal brachial plexus injury surgery. A. The brachial plexus is found in the neck above the clavicle. B. The damaged segment and the level of injury are identified in surgery. C and D. The damaged segment is removed, then reconstructed by taking nerve graft segments from the leg and cabling them to match the size of the damaged nerve. E and F. The cabled nerve graft is sewn in place using microsurgery, allowing the nerve to regenerate to restore function to the paralyzed muscles.
Having a multidisciplinary team allows for surgical reconstruction that is tailored to the individual patient's needs — nerve surgery, tendon transfers and shoulder-to-hand reconstruction — when necessary. Dr. Shin notes that brachial plexus nerve surgery can restore 70 to 80 percent of shoulder and elbow function in certain types of injury. However, imbalances in growth from nerve injury around the shoulder can lead to secondary sequelae: typically, internal retraction contracture and the inability to externally rotate the shoulder.
"If those sequelae aren't addressed before about 2 years of age, the child might experience long-term problems, especially with the shoulder," Dr. Shin says. About 70 to 80 percent of patients who need secondary surgery have good outcomes.
"A baby having a brachial plexus injury can understandingly be an emotional experience for parents," Dr. Shin says. "Our brachial plexus team works together so that parents and baby can move forward with the best possible care."