July 25, 2024
Mayo Clinic applies the latest technical advancements to maximize the safety and outcomes of brain tumor resections. "We continue to innovate to create individualized treatment plans for our patients," says Richard W. Byrne, M.D., chair of Neurologic Surgery at Mayo Clinic in Florida. "We want to meet all our patients' needs — every aspect of treatment and quality of life."
As a designated comprehensive cancer center, Mayo Clinic has neurosurgeons with experience and expertise in all elements of brain tumor care. The Mayo Clinic Brain Tumor Program includes teams specializing in brain metastases, gliomas, meningiomas, pituitary tumors and skull base tumors.
"We often treat people with stage 3 or 4 or metastatic brain cancer. Our expertise allows us to resect tumors that other centers might not," Dr. Byrne says.
Technology that enhances safety and care
Mayo Clinic has pioneered the use of minimally invasive procedures for brain tumor treatment. As a result, many patients leave the hospital within a day or two of tumor surgery and have shortened recovery times.
 Minimally invasive tumor resection
Minimally invasive tumor resection
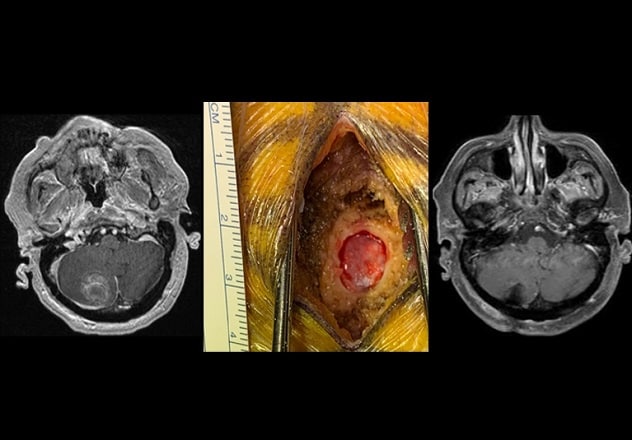
On the left, preoperative MRI shows a large cerebellar metastatic tumor. In the center, photograph shows the burr hole, measuring less than 14 millimeters, through which the tumor was resected. On the right, postoperative MRI shows complete resection. The patient went home on the day following the procedure.
Exoscopic visualization allows Mayo Clinic neurosurgeons to resect certain tumors using a burr hole approach. "We have been able to resect select tumors through a 14-millimeter burr hole, similar to what is used for a needle biopsy," says Kaisorn L. Chaichana, M.D., a neurosurgeon at Mayo Clinic's campus in Florida. "This approach represents the extreme boundary of keyhole surgery. Blood loss is much lower than with conventional surgery. Patients generally go home the following day and recover much faster."
Laser interstitial thermal therapy can be used to treat tumors that are radiation resistant or located in areas difficult to treat, such as the thalamus. Mayo Clinic was an early adopter of this technology.
"Our expertise allows us to resect tumors that other centers might not."
 New construction
New construction
Artist's rendering of the integrated oncology facility under construction at Mayo Clinic in Jacksonville, Florida.
Stereotactic radiosurgery, which delivers precisely focused radiation beams to tumors, is another minimally invasive treatment option. Proton beam therapy provides particular precision and will be offered at the new integrated oncology facility under construction at Mayo Clinic's campus in Florida.
"Proton therapy allows us to deliver higher doses of radiation while minimizing damage to surrounding brain tissue," says Alfredo Quinones-Hinojosa, M.D., a neurosurgeon at Mayo Clinic's campus in Florida. "Proton beam therapy in the hippocampus reduces the likelihood of cognitive and memory deficits. For tumors near the temporal lobe, such as a vestibular schwannoma, there are fewer issues with hearing loss after radiation."
The new oncology center also will include a carbon ion treatment facility. Carbon ion therapy — currently available at only a handful of centers in Asia and Europe — can kill cancer cells that are resistant to traditional radiation therapy.
"Like proton beam therapy, carbon ion therapy minimizes the radiation dose delivered to adjacent normal tissue. We are entering a new era with great potential for treating brain tumors," Dr. Quinones-Hinojosa says.
Awake craniotomy
Mayo Clinic is one of the few centers in the United States that offers awake brain tumor surgery. The procedure helps guide the surgical approach and lower the risk of morbidities.
"Protocols for awake craniotomy exist from the 1930s. It's not new. It's just better and safer now," Dr. Byrne says. "Patients tolerate it remarkably well. For surgeons, awake craniotomy provides instant feedback. You know that what you're doing is safe."
Mayo Clinic researchers found that awake craniotomy performed by a dedicated team is associated with cost savings and reduced hospital stays. As described in JAMA Network Open in January 2024, Mayo Clinic's standardized protocol for awake craniotomy was associated with a mean savings of $7,089 compared with awake craniotomy performed without the standardized protocol.
"Our experience highlights important lessons learned from our awake craniotomy program that allowed for some patients to bypass the ICU, with same-day discharge," Dr. Quinones-Hinojosa says. "For appropriately selected patients, awake craniotomy has significant advantages."
Artificial intelligence
Mayo Clinic is at the forefront of applying artificial intelligence to neurosurgery. As described in the Journal of Neuro-Oncology in September 2022, Mayo Clinic researchers developed a deep learning model that can distinguish MRI indications of tumor progression from pseudoprogression in individuals with glioma. Another deep learning model, described in the January 2023 issue of Biomedical Optics Express, provides real-time, intraoperative delineation of cancer and noncancer brain tissues.
"Artificial intelligence will provide a good portion of future innovations in healthcare," Dr. Byrne says. "That's the case not just in knowledge-based fields but certainly in technical and interventional fields like neurosurgery."
As a major neurosurgical center, Mayo Clinic has the breadth of experience and expertise to provide personalized treatment. "The goal is always to care for the whole patient," Dr. Byrne says. "That means not only maximizing tumor removal but also maintaining quality of life."
For more information
Mayo Clinic Comprehensive Cancer Center. Mayo Clinic.
Brain Tumor Program. Mayo Clinic.
Moniz-Garcia D, et al. Awake craniotomy program implementation. JAMA Network Open. 2024;7:e2352917.
Moassefi M, et al. A deep learning model for discriminating true progression from pseudoprogression in glioblastoma patients. Journal of Neuro-Oncology. 2022;159:447.
Wang N, et al. Deep learning-based optical coherence tomography image analysis of human brain cancer. Biomedical Optics Express. 2023;14:81.
Refer a patient to Mayo Clinic.