Aug. 30, 2019
Compressive and inflammatory myelopathies have diverse etiologies that are often overlooked. As a tertiary center with extensive spinal expertise, Mayo Clinic is able to give most patients more-specific and accurate diagnoses, reducing the risk of disability and of complications due to inappropriate treatment.
"We've shown that in about 70% of cases, we are able to find a cause and get the patient onto the right treatment plan," says Eoin P. Flanagan, M.B., B.Ch., a neurologist at Mayo Clinic in Rochester, Minnesota. That finding, based on a review of idiopathic transverse myelitis cases referred to Mayo Clinic from 2010 to 2015, was published in the Jan. 9, 2018, issue of Neurology.
Mayo Clinic's diagnostic expertise is supported by the enterprise's innovative spinal cord imaging and antibody testing. "The imaging patterns of various myelopathies that have been found by our researchers are extremely helpful when assessing patients. An analysis of cerebrospinal fluid and serum for certain antibodies — some of them discovered at Mayo — can also help establish if the cause is related to an inflammatory process," says Alfonso (Sebastian) S. Lopez Chiriboga, M.D., a neurologist at Mayo Clinic in Jacksonville, Florida.
All three Mayo Clinic campuses use a multidisciplinary approach that involves neurosurgeons and other specialists to provide patients with a diagnosis and treatment plan within a matter of days.
"Optimal patient outcomes can be achieved when there is rapid recognition that the clinical problem is a myelopathy, followed by use of a comprehensive algorithmic approach to diagnosis," says Dean M. Wingerchuk, M.D., a neurologist at Mayo Clinic in Phoenix/Scottsdale, Arizona. "Categorizing the problem as compressive, inflammatory, infectious or related to another cause is an essential step toward a more specific diagnosis and an appropriate treatment plan."
Efficient, multidisciplinary care
Pattern characteristic of cervical spondylotic myelopathy with enhancement
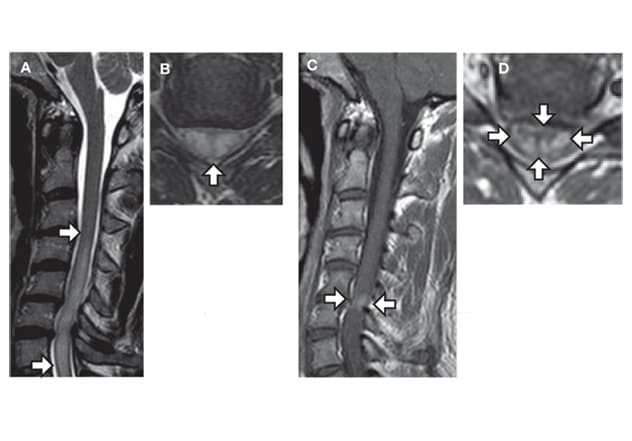
Pattern characteristic of cervical spondylotic myelopathy with enhancement
MRIs show a pattern characteristic of cervical spondylotic myelopathy with enhancement. A. MRI shows a sagittal T2-hyperintense lesion (arrows). B. Central T2-signal (arrow) is visible on the axial image. C. and D. MRI post-gadolinium shows enhancement that forms a transverse band (arrows) with equal width and height, and a pancake appearance — suggesting the sparing of gray matter.
Pattern characteristic of spinal cord sarcoidosis
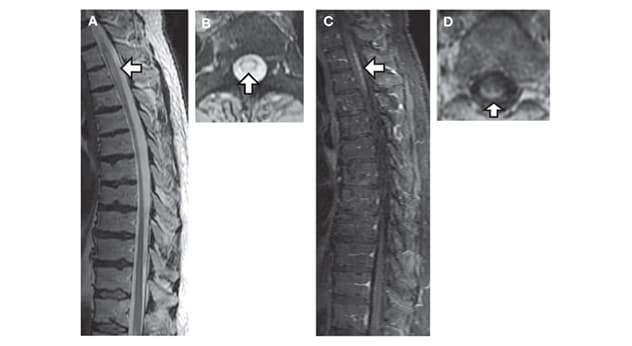
Pattern characteristic of spinal cord sarcoidosis
MRIs show a pattern characteristic of spinal cord sarcoidosis. A. MRI shows a sagittal T2-hyperintense lesion (arrow) in the thoracic spinal cord. B. Central T2-signal (arrow) is visible on the axial image. C. and D. MRI post-gadolinium shows enhancement in the dorsal subpia that has a trident appearance on axial images.
As a fully integrated center, Mayo Clinic coordinates patients' appointments across specialties. A multidisciplinary team reviews any outside imaging and might order additional MRI investigations. Mayo Clinic has published several studies describing unique imaging patterns associated with various myelopathies, including spondylosis, spinal dural arteriovenous fistula (dAVF), spinal cord sarcoidosis and neuromyelitis optica spectrum disorders.
"We've recognized imaging patterns in hundreds of patients who come to us with unusual presentations. Based on that experience, imaging often guides us in the direction of additional testing and evaluations," Dr. Flanagan says. "For example, if we suspect sarcoidosis, we might pursue a CT scan of the chest and bring in our pulmonary colleagues."
Mayo Clinic has also pioneered antibody testing for the diagnosis of inflammatory myelopathies, including the first test available in the United States to identify the myelin oligodendrocyte glycoprotein (MOG) antibody in patient serum. The MOG antibody can distinguish a spectrum of autoimmune demyelinating diseases from multiple sclerosis.
Diseases associated with the MOG antibody and with the aquaporin-4 (AQP4) antibody — also discovered at Mayo Clinic — are commonly misdiagnosed as multiple sclerosis. "Detection of one of these antibodies at first presentation not only allows for specific early diagnosis but also the development of a preventive treatment plan, because the antibody profile contributes to our ability to predict whether a patient is likely to have future relapses," Dr. Wingerchuk says.
Autoimmune testing is performed by Mayo Clinic Laboratories. "Our experience with this testing means we avoid mistakes that sometimes occur, such as performing testing after a plasma exchange, which can lead to a false-negative result," Dr. Flanagan says. "Our lab can perform these tests and provide results usually within a week."
Accurate diagnosis is essential to prevent complications. For example, the steroids prescribed to treat inflammatory myelopathy can lead to profound disability for people who actually have a spinal dAVF.
"We also see patients who were put on immunosuppressant medications for a suspected inflammatory myelopathy who ultimately received an alternative diagnosis that did not require administration of immunotherapy. Achieving a specific diagnosis is crucial, as chronic immunosuppression can lead to serious infections," Dr. Lopez says.
Once the cause of an idiopathic myelopathy is correctly identified, Mayo Clinic's multidisciplinary team can provide treatment. "We work closely with our neurosurgeons in cases of a vascular or spondylotic myelopathy," Dr. Flanagan says. "Treatment outcomes from myelopathies can be good, depending on the cause and when appropriate treatment is initiated. If there is any uncertainty about the cause of myelopathy, a referral to Mayo Clinic can result in an accurate diagnosis and intervention that will prevent harm."
For more information
Zalewski NL, et al. Evaluation of idiopathic transverse myelitis revealing specific myelopathy diagnoses. Neurology. 2018;90:e96.