March 01, 2019
As a fully integrated tertiary medical center, Mayo Clinic provides a comprehensive team approach to endoscopic skull base surgery. At all three Mayo Clinic campuses, neurosurgeons, neurologists, endocrinologists, otolaryngologists and neuro-ophthalmologists collaborate at each step, from preoperative workup through surgery and postoperative care.
"The Mayo Clinic Model of Care is ideal for endoscopic skull base surgery. Patients are best served when they see all of these specialists throughout the process," says Bernard R. Bendok, M.D., chair of Neurosurgery at Mayo Clinic in Phoenix/Scottsdale, Arizona. "This is where team medicine shines."
Mayo Clinic specialists have extensive experience with endoscopic skull base surgery for the treatment of pituitary tumors, meningiomas, clival tumors, chordomas and craniopharyngiomas. Occasionally, the procedure is used to treat certain cavernomas and aneurysms.
Endoscopic skull base surgery can also be combined with proton beam therapy, an approach that can be particularly helpful for the treatment of chordomas. For most patients with pituitary tumors and chordomas, Mayo strives to optimize resection before beginning radiation therapy if that therapy is needed.
Pituitary tumor compressing the optic nerve

Pituitary tumor compressing the optic nerve
MRI of a 65-year-old man shows a pituitary tumor compressing the optic nerve. The patient had experienced a worsening visual deficit in his right eye before being referred to Mayo Clinic.
Near-blindness in the right eye

Near-blindness in the right eye
An optometry exam found near-blindness in the right eye, as shown by the dark areas in the right-hand image.
Pituitary tumor after endoscopic skull base surgery

Pituitary tumor after endoscopic skull base surgery
MRI performed a year after endoscopic skull base surgery at Mayo Clinic illustrates treatment of the pituitary tumor.
Vision restored after the tumor resection
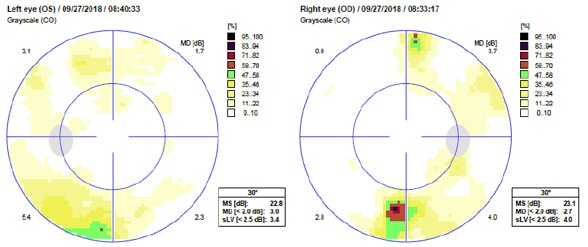
Vision restored after the tumor resection
An optometry exam one year after surgery shows the restoration of vision after the tumor resection.
"That's a very important point that isn't always considered," Dr. Bendok says. "Skull base tumors can be located near critical radiation-sensitive structures, including the optic nerves. When a tumor cannot be removed completely, creating space between the residual tumor and the optic nerves can be a worthwhile surgical goal to reduce potential injury to vision. To obtain the optimal surgery, patients should ask how close their tumors are to the optic chiasm and how the surgical team will manage that."
Maximizing safety during surgery
Mayo Clinic uses sophisticated imaging to enhance the safety of endoscopic skull base surgery, including holography and augmented reality. Both techniques are used preoperatively to visualize and plan the procedure; holography is also used for intraoperative visualization.
"Our visualization in health care to date has been two-dimensional," Dr. Bendok says. "But holography takes 3D to the next level. It allows everyone in the operating room to understand what's happening. The enhanced visualization helps the surgeon to perform an optimal surgery."
Intraoperative CT, MRI and angiography are also key to enhancing safety while providing optimal resection. Mayo Clinic will soon have a hybrid system for intraoperative neurological CT and MRI.
"This is a highly sophisticated operating room with a robotic C-arm that allows us to perform intraoperative CT and then slide the patient over and do intraoperative MRI right next door. It's very unique," Dr. Bendok says. "Having CT and MRI, as well as intraoperative angiography, allows us to assess our skull base work with intraoperative and robotic fluoroscopy and to get quick control of the carotid arteries and other vessels if necessary during surgery."
To reduce the risk of stroke, Mayo Clinic uses balloon test occlusion for high-risk patients, such as those who have had prior radiation or previous surgery. Through the use of nasoseptal or other ancillary flaps for skull base repair, Mayo Clinic has achieved negligible rates of postoperative cerebrospinal fluid leak.
For postoperative care, Mayo Clinic has a neuroscience intensive care unit (ICU) if needed — although most patients can move to a surgical-ward room after endoscopic skull base surgery. "As the surgery has become less invasive, we've been able to move away from using the ICU for most of these patients," Dr. Bendok says.
The team approach continues outside the operating room. Endocrinologists evaluate patients postoperatively in the hospital and again at visits within two weeks of surgery. "If the patient has a local endocrinologist, there is a handoff, with the Mayo skull base team sending a full report," Dr. Bendok says.
"The pillars that support our skull base surgery practice are the various specialties that work synergistically with our neurosurgeons," he adds. "Our commitment to that very close integration is the strength we offer to patients."