Aug. 20, 2021
Mayo Clinic uses both positron emission tomography (PET) scans and 7-tesla MRI to image individuals with epilepsy to identify potential candidates for surgical treatment.
"We see PET and 7-tesla MRI as complementary. Together they offer a wider range of information that increases our likelihood of detecting small epileptogenic lesions," says Steven A. Messina, M.D., a neuroradiologist at Mayo Clinic in Rochester, Minnesota. "Having both PET and 7-tesla MRI in our armamentarium is quite unique."
Approximately one-third of individuals with epilepsy have medically refractory seizures and might benefit from surgery if epileptogenic lesions are identified.
"We're now finding lesions in people with epilepsy that low-field imaging didn't uncover. Having these clear targets helps us intervene for better reduction or cure for seizures in patients," says Kai J. Miller, M.D., Ph.D., a neurosurgeon at Mayo Clinic's campus in Minnesota.
Metabolic abnormality associated with seizure origin
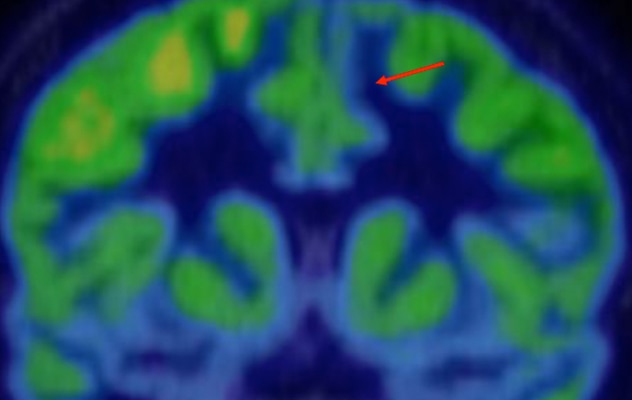
Metabolic abnormality associated with seizure origin
Positron emission tomography scan demonstrates hypometabolism (red arrow) at the site of a suspected left frontal lobe lesion.
Patients referred to Mayo Clinic have initial PET scans and 3-tesla MRI. If those tests indicate metabolic abnormalities associated with seizure-origin sites as well as potential suspect lesions, 7-tesla MRI is performed.
"The findings on the PET help guide us in reviewing the 7-tesla MRI to identify a possible seizure-origin site," Dr. Messina says. "The 7-tesla MRI provides increased resolution of the underlying brain tissue, which is a definite advantage when trying to identify subtle lesions related to focal epilepsy."
3-tesla MRI of epileptogenic lesion
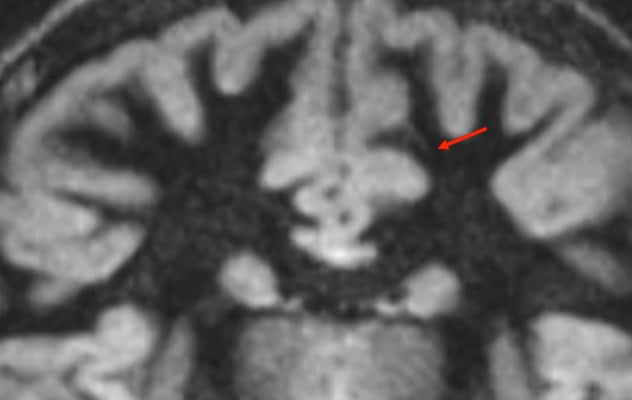
3-tesla MRI of epileptogenic lesion
This 3-tesla MRI shows faint indications of an epileptogenic lesion, compatible with focal cortical dysplasia (red arrow).
7-tesla MRI of epileptogenic lesion
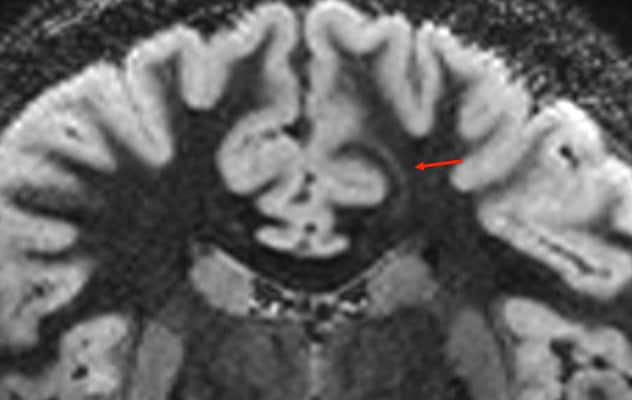
7-tesla MRI of epileptogenic lesion
This 7-tesla MRI provides a clear view of the epileptogenic lesion (red arrow).
Mayo Clinic was the first center in North America to use clinical 7-tesla MRI, after the system was approved in 2017. For comparison, 7-tesla provides a magnetic field more than three times stronger than conventional 3-tesla MRI.
"Between 20% and 30% of the lesions we detect with 7-tesla MRI are lesions that we're not able to detect with 3-tesla MRI," Dr. Messina says. "The high magnetic field strength of 7-tesla MRI can produce artifacts that can obscure some anatomical regions typically involved with epilepsy, particularly the temporal lobes. But our neuroradiologists are working closely with our Mayo Clinic physicists to develop techniques to mitigate these limitations and avoid the artifacts that affect the interpretation of temporal lesions."
Mayo Clinic's efforts to improve the detection of epileptogenic lesions include clinical studies involving 7-tesla MRI. One study focuses on the ability of 7-tesla MRI to detect very small lesions. A second study is evaluating hippocampal volumetric software used with 7-tesla MRI to assess individuals with epilepsy.
"We continue to push the limits of what we can do with our current technology," Dr. Messina says. "Our goal is to identify every possible candidate for epilepsy surgery, to potentially improve their chances of seizure freedom."