Sept. 21, 2021
Evolution of lesions
Evolution of lesions
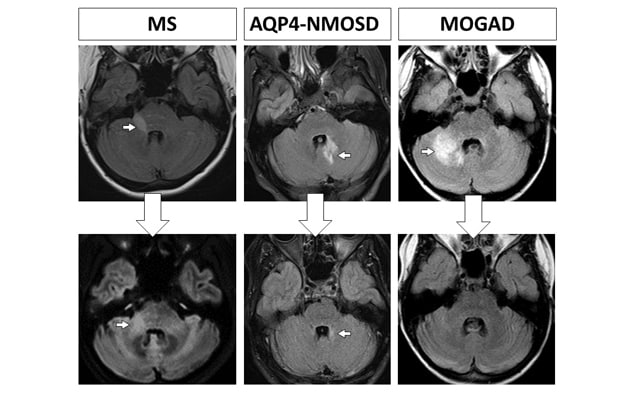
In the top row, brain MRI scans show lesions (arrows) occurring during an attack of multiple sclerosis (MS), aquaporin-4-IgG-positive neuromyelitis optica spectrum disorder (AQP4-IgG-NMOSD) and myelin-oligodendrocyte-glycoprotein-IgG-associated disorder (MOGAD). In the bottom row, follow-up MRI performed months to years later shows the moderately sized scar left by the MS lesion (arrow) and the small scar left by the AQP4-IgG-NMOSD lesion (arrow). The follow-up MOGAD scan shows complete resolution of the lesion.
Mayo Clinic researchers have identified clear differences in the evolution of lesions in individuals with certain demyelinating diseases. As described in a study to be published in Neurology, the findings can potentially inform the diagnosis and treatment of multiple sclerosis (MS), myelin-oligodendrocyte-glycoprotein-IgG-associated disorder (MOGAD) and aquaporin-4-IgG-positive neuromyelitis optica spectrum disorder (AQP4-IgG-NMOSD).
The study compared the results of T2-weighted MRI performed on Mayo Clinic patients with demyelinating diseases at the time of acute attacks and six months later. The researchers found that lesions resolved completely more frequently in individuals with MOGAD than in patients with MS or AQP4-IgG-NMOSD.
"The differences in lesion evolution that we found will help physicians distinguish these three diseases more easily to aid in diagnosis," says Eoin P. Flanagan, M.B., B.Ch., a neurologist at Mayo Clinic in Rochester, Minnesota. "More importantly, our findings improve our understanding of the mechanisms of nerve damage in these three diseases and may suggest an important role of such lesions in the development of long-term disability in MS."
In patients with MS, the researchers found only a moderate reduction in MS lesion size — typically 30% to 70% — on MRI six months after an attack compared with MRI at the time of attack. Although MS is characterized by smaller lesions and less severe attacks compared with other demyelinating diseases, MS lesions are known to persist over time despite the resolution of clinical MS features.
"We believe that the persistence of these lesions in MS, particularly larger lesions in critical locations, might over time represent a nidus for secondary disability progression," Dr. Flanagan says. "The tendency of some MS lesions to remain chronically active between relapses — so-called smoldering MS lesions — could support this hypothesis. Reports of progressive disability attributable to a single persistent, large lesion in an eloquent location that becomes focally atrophic over time are also consistent with this hypothesis."
Elucidating rare demyelinating diseases
The evolution of MOGAD and AQP4-IgG-NMOSD lesions has been studied much less than MS lesions. Mayo Clinic's research provides insight into the clinical progression seen in individuals with these less common demyelinating diseases.
The tendency of MOGAD lesions to resolve completely at follow-up — despite their large size and the severe clinical impairment that initially accompanies them — is in line with the favorable long-term outcomes experienced by most patients with MOGAD.
"These patients tend to generally do well in the long term despite their severe attacks. They don't experience the gradual disease progression that we frequently encounter with MS," Dr. Flanagan says.
Compared with MOGAD lesions, the lesions associated with AQP4-IgG-NMOSD are of similar size and accompanying clinical severity. But unlike MOGAD lesions, AQP4-IgG-NMOSD lesions rarely resolve completely. The Mayo Clinic study found that, although AQP4-IgG-NMOSD lesions are generally reduced by 60% to 80% six months after an attack, small regions of residual T2-hyperintensity are usually evident.
"That finding is consistent with the incomplete recovery and stepwise, attack-related disability that accumulates in AQP4-IgG-NMOSD," Dr. Flanagan says.
He notes that the mechanism behind the generally complete resolution of MOGAD lesions is unclear. "It would be helpful for us to better understand that process, and also to know more about why MS lesions don't recover as well," Dr. Flanagan says. "That improved understanding could be a first step toward an ultimate goal of developing treatments to help MS lesions also resolve."
For more information
Sechi E, et al. Comparison of MRI lesion evolution in different central nervous system demyelinating disorders. Neurology. In press.