Jan. 26, 2024
Mayo Clinic uses 7T MRI for enhanced visualization of cerebral cavernous malformations, facilitating optimal management of these vascular abnormalities.
"The 7-tesla magnet gives us significantly greater definition of a cavernous malformation. We are able to better understand the anomalous venous structures often associated with a malformation — which are probably, in many cases, the malformation's cause," says Giuseppe Lanzino, M.D., a neurosurgeon at Mayo Clinic in Rochester, Minnesota.
Indeed, using 7T MRI, Mayo Clinic researchers have found that the prevalence of anomalous venous structures might be much higher than previously thought. The researchers set out to evaluate the prevalence of developmental venous anomalies in individuals who presented with sporadic cavernous malformations.
 Cavernous malformation on 7T MRI
Cavernous malformation on 7T MRI
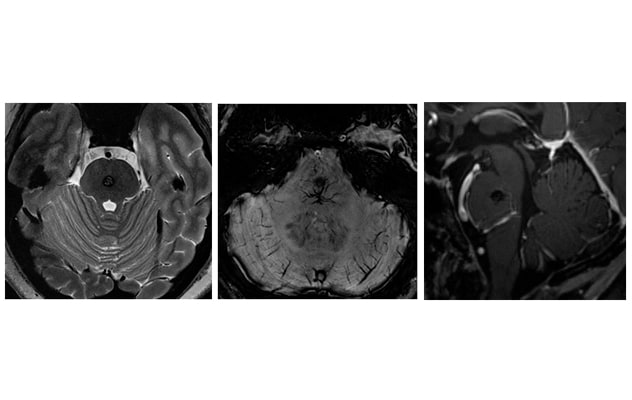
On the left, axial T2-weighted 7T MRI shows a cavernous malformation in the central pons. In the center and on the right, axial susceptibility-weighted imaging and sagittal post-contrast T1-weighted 7T MRI show an adjacent developmental venous anomaly along the inferior aspect of the cavernous malformation.
"Using high-quality 7-tesla imaging, 72% of patients with a sporadic cavernous malformation were found to have an associated developmental venous anomaly," says Petrice M. Cogswell, M.D., Ph.D., a neuroradiologist at Mayo Clinic's campus in Minnesota. "An associated anomaly was most common for cavernous malformations in the brainstem compared with the cerebral hemispheres or cerebellum."
7T MRI can distinguish cavernous malformations from other types of brain disease. The advanced imaging technology also enhances decision-making about treatment, bolstering Mayo Clinic's expertise with this complex condition.
"Cavernous malformations are challenging because there's often a substantial risk of bleeding — but also risks associated with surgical removal, especially when malformations are located in highly eloquent areas of the brain," says Kelly D. Flemming, M.D., a neurologist at Mayo Clinic's campus in Minnesota. "We have a multidisciplinary team with experience in the natural history and outcomes of cavernous malformations that works together to evaluate the risks and determine the best management strategy."
Balancing risks
Mayo Clinic has been designated a Center of Excellence for cavernous malformation treatment and research by the Alliance to Cure Cerebral Cavernous Malformation, a patient advocacy group. As a fully integrated center, Mayo Clinic coordinates appointments across specialties. "Usually, a patient can have all the imaging and appropriate consultations done and receive a treatment plan within two days," Dr. Flemming says.
Patients with cavernous malformations are often young adults or sometimes children. A malformation might be asymptomatic and found incidentally, or a patient might present with bleeding, focal neurological deficits, headaches or seizures.
"These seizures can be quite difficult to control with medication. That might be an indication for surgery," Dr. Lanzino says.
Cavernous malformations have a less than 2% annual risk of clinically significant hemorrhage. However, once a patient experiences a hemorrhage, there is a 30% to 50% chance of recurrent bleeding over the next five years. While surgery remains the mainstay of treatment, the decision about whether to resect a cavernous malformation that has bled isn't necessarily straightforward.
"There are a lot of misconceptions about cavernous malformations," Dr. Lanzino says. "Although the risk of another bleed is fairly substantial, it's also true that when a cavernous malformation bleeds, the surrounding tissue is often displaced rather than permanently damaged. Patients often improve on their own without any additional treatment, while remaining at substantial risk of additional hemorrhage."
At Mayo Clinic, decisions about the management of a cavernous malformation are made on an individual basis. In addition to subspecialized neurologists, the multidisciplinary treatment team includes experts in neuroradiology, stereotactic radiosurgery and open neurological surgery.
"Usually, a patient can have all the imaging and appropriate consultations done and receive a treatment plan within two days."
"Very particular trajectories and approaches are necessary to reach cavernous malformations, while minimizing as much as possible the risk of damage to surrounding tissue," Dr. Lanzino says. "Our surgeons are well experienced with these various approaches. We also have significant experience with cavernous malformations in areas where lesions were once considered inoperable — such as the brainstem and thalamus — with very good results."
Dr. Lanzino notes that at Mayo Clinic, most patients who present with seizures experience better seizure control after resection of a cavernous malformation. "A significant percentage of these patients can potentially discontinue medication after being seizure-free for 1 to 2 years after surgery," he says.
Future treatment options
Mayo Clinic is at the forefront of cavernous malformations research. Mayo physician-scientists have published research on more than 400 patients in the Mayo Clinic Cavernous Malformation Prospective Registry, an effort to learn more about the condition's natural history and outcomes.
Other efforts include:
- A multicenter effort to develop the infrastructure for clinical trials of new therapeutics for nonsurgical candidates.
- A multicenter study assessing the ability of select blood biomarkers to predict hemorrhage risk.
- Clinical trials assessing the ability of certain medications to prevent bleeding from cavernous malformations.
- Gene therapy for familial cavernous malformations in mouse models of the disease.
"These advances are incredible," Dr. Flemming says. "It's pretty exciting that there may be candidate medications for people who don't want or can't have surgery but also don't want the risk of bleeding from a cavernous malformation."
"At Mayo Clinic, we have made a lot of progress in the past 20 years with cavernous malformations, in terms not only of imaging and diagnosis but also of understanding the natural history and indications for treatment," Dr. Lanzino says. "We bring that experience, and our commitment to the best possible care for our patients."
For more information
Refer a patient to Mayo Clinic.