July 16, 2021
The prevalence of hirsutism has been estimated to be as high as 8% in women in the United States. The evaluation of hirsutism often includes measurement of serum total testosterone (TT) concentrations to determine the need to screen for an androgen-producing tumor (APT). Although prior guidelines generally recommend that TT testing be performed only for women with moderate to severe hirsutism, more-recent guidelines suggest inclusion of all women presenting with concerns for hirsutism.
Taking into account the most common condition of androgen excess, polycystic ovary syndrome, as many as 16% to 20% of premenopausal women in the United States might be tested. Therefore, the endocrinologist in clinical practice is frequently faced with dilemmas of interpretation of degree of testosterone elevation and need for further studies to exclude an APT.
Leydig cell tumor
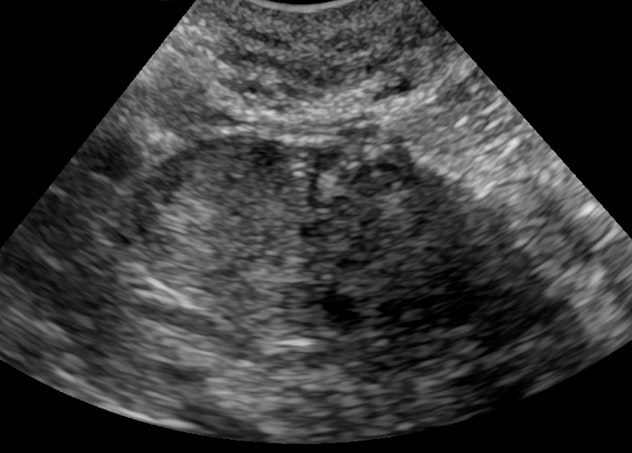
Leydig cell tumor
Pelvic ultrasound shows evidence of Leydig cell tumor in the right ovary.
In postmenopausal women, pathological hyperandrogenism (PH) caused by ovarian hyperthecosis can be even more difficult to diagnose by ovarian imaging alone, yet PH is quite distressing for postmenopausal women who are more likely to present with severe symptoms.
Ravinder J. Singh, Ph.D., Clinical Biochemistry and Immunology and Laboratory Medicine and Pathology, at Mayo Clinic in Rochester, Minnesota, notes: "Previously reported discriminatory thresholds for APT were based on measurements of TT by radioimmunoassays, which are less accurate in women than men. Liquid chromatography with tandem mass spectrometry (LC-MS/MS) provides specific and accurate measurement of TT concentrations and is endorsed as the preferred measurement method by the Endocrine Society."
Dana Erickson, M.D., Endocrinology, Diabetes, Metabolism, and Nutrition, at Mayo Clinic in Minnesota, says: "In a retrospective study published in Clinical Chemistry in 2018, we studied a large group of women who presented with severe biochemical hyperandrogenemia — TT concentration of 100 ng/dl or more — over a 10-year period beginning in 2004, when TT was exclusively measured by LC-MS/MS. We sought to identify the optimal discriminatory threshold for APT by LC-MS/MS."
After exclusion of patients with exogenous hyperandrogenism and patients with adrenocortical carcinoma and Cushing syndrome, findings showed:
- 21 (24%) women were diagnosed with APT
- 16 (18%) women were diagnosed with PH
- 52 (58%) women were diagnosed with polycystic ovary syndrome (PCOS)
Women with APT were more likely to have male-pattern alopecia documented on physical examination (APT 33% vs. PH 19% vs. PCOS 10%, p < 0.05), and the source of the APT was more frequently ovarian (81%, n = 17) than adrenal (19%, n = 4). "We found the duration of time from onset of symptoms to time of presentation in APT was within 1 to 2 years, similar to that previously reported," says Dr. Erickson.
Menstrual history and signs and symptoms of hyperandrogenism were not significantly different between PCOS and AP, although 71% of women with APT were either postmenopausal or had already had hysterectomies.
TT concentrations were significantly higher in the APT group than in women with PCOS or PH. After receiver operating characteristic (ROC) curve analysis, a TT concentration of 148 ng/dl (5.1 nmol/L) or greater had a sensitivity of 90% and specificity of 81% for the diagnosis of APT (AUC, 0.90).
Eighty-one women received at least one imaging study, and 18 (22%) were identified as having an APT. Transabdominal or transvaginal ultrasonography (ultrasound) was the first radiologic test obtained in 75 (84%) women; it failed to identify APT in four women. MRI did not identify any tumors that were not already identified.
Three women (one premenopausal and two postmenopausal) required ovarian and adrenal vein sampling to diagnose an ovarian source.
Alice Y. Chang, M.D., Endocrinology, Diabetes, Metabolism, and Nutrition, at Mayo Clinic in Minnesota, adds: "We also performed a secondary analysis that included all postmenopausal women presenting with symptoms or signs of hyperandrogenism during the same time period. This analysis assessed 71 women, including 20 from the first cohort, with the hypothesis that given the significant decline in ovarian androgen production after menopause, the diagnostic threshold would be lower for PH in postmenopausal women — PH defined as either APT or ovarian hyperthecosis."
Serum total testosterone levels

Serum total testosterone levels
Serum total testosterone levels in postmenopausal women with symptoms of hyperandrogenism. IH: idiopathic hyperandrogenism; PH: pathological hyperandrogenism.
The researchers identified 36 women with idiopathic hyperandrogenism and 35 women with PH. Results included:
- ROC analysis of TT concentrations revealed the most optimal diagnostic threshold was 64 ng/dl (2.2 nmol/L, sensitivity 100%; specificity 86%) or greater for the diagnosis of PH (AUC, 0.95).
- Out of the 35 women in the PH group, 20 (57%) had a clinical or pathological diagnosis of ovarian hyperthecosis and 15 (43%) met the criteria for an APT.
- Of those with a diagnosis of ovarian hyperthecosis, median ovarian volumes on pelvic ultrasound were 4.3 mL (3.0 to 4.8 mL) on the right and 5.3 mL (2.0 to 12 mL) on the left. "These results could be reported as normal by the radiologist," says Dr. Chang.
- Of the women with ovarian hyperthecosis, 11 (52%) received bilateral oophorectomy.
- Pathological diagnoses were either bilateral stromal hyperplasia in five women (45%) or no identified diagnostic abnormality in six women (55%). "The diagnoses highlight that ovarian hyperthecosis can be difficult to diagnose by both imaging and pathology," notes Dr. Chang.
- In those without imaging or pathological abnormality (n = 6), postoperative testosterone concentrations were all within the normal range, with resolution of hyperandrogenism symptoms on follow-up.
"Given the predicted shift of all TT measurements to LC-MS/MS in women, these results provide an important update to clinical practice," says Dr. Erickson. "Consideration should be given to using a lower diagnostic threshold for TT measured by LC-MS/MS in the evaluation of women with suspected APT. An even lower diagnostic threshold should be considered in postmenopausal women for the identification of pathological causes of postmenopausal hirsutism, including both APT and ovarian hyperthecosis."
For more information
Sharma A, et al. Diagnostic thresholds for androgen-producing tumors or pathologic hyperandrogenism in women by use of total testosterone concentrations measured by liquid chromatography-tandem mass spectrometry. Clinical Chemistry. 2018;64:1636.