June 09, 2018
Heterotopic ossification (HO) — the formation of bone outside the normal skeleton — can occur in soft tissue and is usually found within muscular, adipose, or nonmuscle fibrous or connective tissue. Ectopic bone formation is the only example of complete recapitulation of an organ system, replete with hard tissue, vascular and marrow elements.
Robert J. Pignolo, M.D., Ph.D., with Geriatric Medicine and Gerontology and Endocrinology, Diabetes, Metabolism, and Nutrition at Mayo Clinic's campus in Rochester, Minnesota, says: "Genetic forms of HO, such as fibrodysplasia ossificans progressiva (FOP), primary osteoma cutis (OC), progressive osseous heteroplasia (POH), pseudohypoparathyroidism (PHP) and Albright's hereditary osteodystrophy (AHO)-pseudopseudohypoparathyroidism (PPHP), can be progressive soon after birth and throughout life.
"In contrast, nonhereditary heterotopic ossification (NHHO) tends to be limited and usually arises in the context of trauma or certain arthropathies or following injury that is often sustained in the context of age-related pathology, although these categories are not mutually exclusive.
"Central nervous system, musculoskeletal, cutaneous and vascular injury predispose an individual to ectopic bone formation, and NHHO occurs as a clinically severe complication in as many as approximately 20 percent of all individuals following major hip surgery, and in as many as approximately 11 percent of those following traumatic brain injury. Bone formation limited to ligaments may occur with seronegative spondyloarthropathies or diffuse idiopathic skeletal hyperostosis.
"NHHO may be found in age-related conditions, particularly in the context of common vascular pathology, as well as after total hip arthroplasty for age-onset degenerative joint disease. End-stage calcific valvular heart disease is prevalent in advanced age, and HO occurs in up to 13 percent of patients with this diagnosis. Age-related HO can occur in a variety of other conditions associated with immobilization, such as neuromuscular disorders, or in the context of clinical factors common in the geriatric population, such as pressure sores, urinary tract infection or trauma."
In a patient presenting with HO, nonhereditary forms can usually be excluded on the basis of prior trauma or surgery, age, and known history or suspicion of arthropathy. Dr. Pignolo explains: "Among genetic forms of HO, FOP is distinguished by the cardinal features of congenital malformation of the first toes and pre-osseous tumorlike inflammation or flare-ups."
Diagnostic algorithm for distinguishing PHP
Diagnostic algorithm for distinguishing PHP
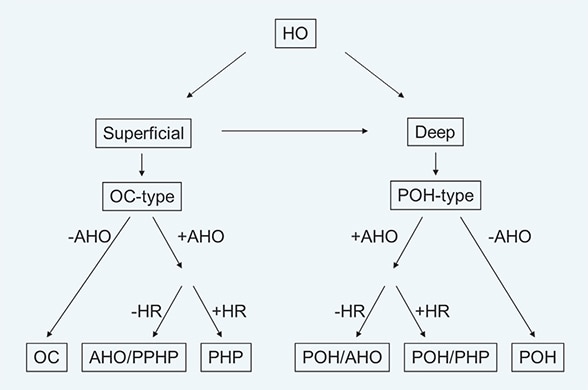
Diagnostic algorithm for distinguishing among PHP and related conditions of heterotopic ossification. Abbreviations used: AHO, Albright's hereditary dystrophy; HO, heterotopic ossification; HR, hormone resistance; OC, osteoma cutis (primary); PHP, pseudohypoparathyroidism; POH, progressive osseous heteroplasia; and PPHP, pseudopseudohypoparathyroidism.
PHP and related disorders (primary OC, POH, AHO-PPHP) can be distinguished on the basis of three characteristics:
- Extent of HO (superficial or deep; predominantly intramembranous ossification)
- AHO features (more than two features, especially brachydactyly, but also short stature, obesity, round face and neurobehavioral abnormalities)
- Hormone resistance, especially elevated parathyroid hormone (+/- hypocalcemia and hyperphosphatemia), but also elevated thyroid-stimulating hormone and hypothyroidism, hypogonadism, elevated calcitonin and growth hormone deficiency. This approach is primarily clinical.
Dr. Pignolo continues: "In the case of genetic forms of HO, the ultimate clinical diagnosis will be supported by associated features of the specific condition and molecular confirmation of involvement of known genes. Consideration should be given to the age at presentation before a definitive diagnosis is made, since there tends to be a sequence in both biochemical and osseous progression. Exclusion of genetic etiologies, based on older age at presentation alone, should be carefully considered.
"After the clinical diagnosis is established, screening for the molecular cause should be performed for confirmation of the diagnosis and further characterization of the subtype of the disease. The decision for molecular diagnosis and on its type should be based on clinical characteristics and local access to genetic analyses. The specific genotyping should consider the most frequently identified causes of the disease at the time of analysis — for instance, GNAS, ± PRKAR1A sequencing and ± analysis of the GNAS differentially methylated regions in PHP1A."