May 24, 2016
Ischemic cerebrovascular events such as stroke and transient ischemic attack (TIA) are the most feared complications of cardiovascular disease. They are a focus of concern for all patients, and for physicians and health care providers, they often represent a conundrum in both diagnosis and treatment:
- Is the TIA a result of paradoxical embolus across a patent foramen ovale (PFO)?
- Is the embolic stroke caused by a thrombus in the left atrial appendage (LAA) in an individual with atrial fibrillation (AF)?
Establishment of a cause-and-effect relationship frequently is difficult but affects diagnostic and treatment strategies made even more problematic because some patients have multiple coexistent substrates.
To address these issues and as a logical development of team-based care, Mayo Clinic in Rochester, Minnesota, has created the Heart Brain Clinic, which provides multidisciplinary evaluations to individuals who have had neurological symptoms that may be attributable to a cardiac etiology such as PFO or AF. Specialists from the Division of Cardiovascular Diseases and the Division of Stroke and Cerebrovascular Disease in the Department of Neurology collaboratively evaluate patients, directing further evaluation, educating patients and families, and making a joint recommendation for management.
Atrial fibrillation
Atrial fibrillation is associated with up to 20 percent of strokes, particularly in older patients. This incidence may be even higher in patients who have silent short episodes of AF.
Although anticoagulation has been found to be effective for stroke prevention, it may not be prescribed or used in up to 50 percent of patients at risk. Indeed, in patients at highest risk of stroke, the use of routine anticoagulation may be even less because of various clinical and patient issues and concerns.
The role of LAA thrombus in the pathophysiology of stroke in patients with nonvalvular AF has long been recognized. Based on autopsy and echocardiographic studies, the vast majority of strokes in these individuals are believed to be embolic in nature. LAA thrombus formation in AF may be related to the anatomy of the left atrium and pectinate muscles, inflammation, and fibrosis, hence the interest in developing site-specific therapy such as LAA occlusion, with either percutaneous devices or ligation.
The appeal of these approaches is greatest in those patients for whom chronic anticoagulation poses special risks. Standard anticoagulation regimens may be problematic in individuals prone to falls, those who have had prior brain or systemic hemorrhage, or those with extensive renal or hepatic disease, although these patients may be at high risk of stroke and have the most to gain by stroke prevention.
Also problematic is establishing causality in the individual with ischemic stroke and sinus rhythm, but with suspected or documented paroxysmal atrial fibrillation. The prevalence of AF increases with age, as does the risk of comorbid conditions that also increase the risk of ischemic stroke such as atheromatous carotid or vertebral disease, small artery occlusive disease in the brain, or other cardiac conditions. Therefore, individuals with ischemic stroke and AF benefit from comprehensive evaluation to consider other causes before recommending a specific treatment course.
Patent foramen ovale
MRI and transthoracic imaging are used to identify and characterize PFO
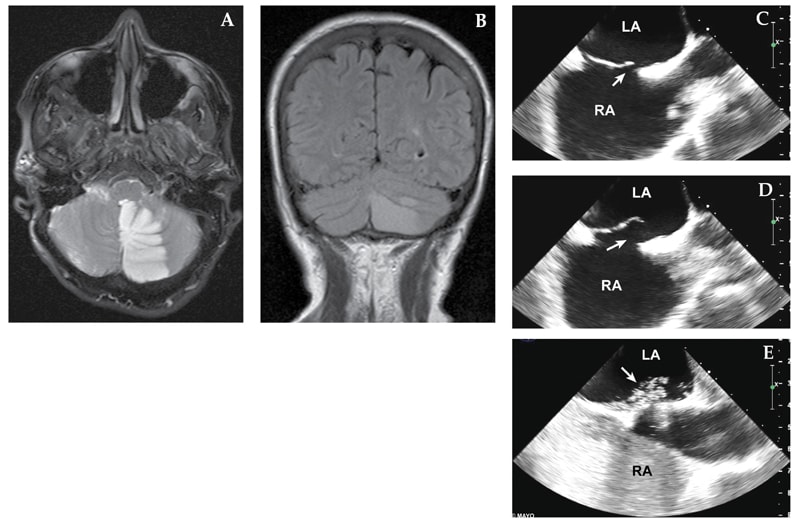
MRI and transthoracic imaging are used to identify and characterize PFO
A 63-year-old woman who had a remote history of migraine awakened with a headache with visual aura, as well as nausea, vomiting and incoordination. She was a former smoker but had no history of hypertension, estrogen replacement or family history of stroke. A and B. MRI demonstrated a left cerebellar infarct. C and D. Transesophageal echocardiography demonstrated a large PFO (arrow) with an atrial septal aneurysm. E. Contrast injection demonstrated generous flow across the PFO (arrow) with Valsalva. Percutaneous closure was performed. LA, left atrium; RA, right atrium.
The prevalence of PFO in the adult general population may be as high as 25 percent; usually these interatrial shunts are asymptomatic and of no hemodynamic importance. Until the advent of echocardiography, it was difficult to diagnose PFO antemortem. Transthoracic imaging, especially with agitated saline contrast injection, transesophageal echocardiography and transcranial Doppler, is widely used to identify and characterize PFO.
Case reports from the echocardiographic literature illustrate venous thrombi straddling PFO, demonstrating the potential for systemic (paradoxical) embolization. Sluggish blood flow and the funnel-shaped interatrial connection created by some PFOs may facilitate the in situ formation of thrombi, and individuals with coagulopathies may be at higher risk.
Given the prevalence of PFO in the overall population and the risk of stroke in older individuals, it is often difficult to definitively attribute stroke to a paradoxical embolus, especially in older patients. However, the association between cryptogenic stroke and PFO is much stronger in younger individuals.
Unfortunately, the available randomized clinical trials have failed to demonstrate clear definitive superiority of any treatment option such as device closure, aspirin or warfarin. Whether this relates to the concurrence of other mechanisms of stroke, of which there are many, or actual failure of the selected treatment strategy is unknown. The effectiveness of the new oral anticoagulants in preventing stroke in patients with PFO has not been evaluated.
Bringing together expertise in cardiovascular diseases and neurology in the same clinical setting allows these complex clinical issues to be seamlessly addressed for patients and their families. After the initial consultations, the multidisciplinary group of caregivers recommends and implements any additional testing and provides a recommendation regarding the optimal management approach.
For more information
To contact the Heart Brain Clinic at Mayo Clinic in Rochester, please call Cardiovascular Diseases at 507-255-4244 or Neurology at 507-284-1588.