Nov. 27, 2019
In the U.S., data show that a stroke occurs every 40 seconds — and every four minutes, a person dies of stroke, accounting for approximately 800,000 stroke deaths a year. Experiencing an initial stroke puts patients at risk for subsequent strokes, further disability and even death.
A collaborative specialty clinic
Preventing subsequent strokes is difficult, particularly when the cause of the first stroke is unknown, as it is in up to one-third of patients who have transient ischemic attacks (TIAs) or cryptogenic strokes. For improved care, a real-time collaborative multidisciplinary diagnostic workup with cardiac and neurology specialists was needed — a heart brain clinic. In 2013, Mayo Clinic opened its first Heart Brain Clinic.
Explains Naser M. Ammash, M.D., a specialist in adult congenital heart disease at Mayo Clinic's campus in Rochester, Minnesota:
Large patent foramen ovale with an atrial septal aneurism requiring percutaneous closure
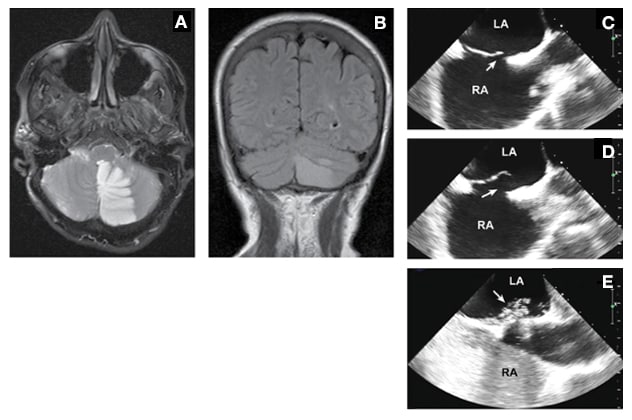
Large patent foramen ovale with an atrial septal aneurism requiring percutaneous closure
A 63-year-old woman with a remote history of migraine awakened with a headache with visual aura, as well as nausea, vomiting and incoordination. She was a former smoker but had no history of hypertension or estrogen replacement and no family history of stroke. A and B. MRI demonstrated a left cerebellar infarct. C and D. Transesophageal echocardiography demonstrated a large patent foramen ovale (arrow) with an atrial septal aneurysm. E. Contrast injection demonstrated generous flow across the patent foramen ovale (arrow) with Valsalva maneuver. Percutaneous closure was performed.
"The idea came to me in 2013 during a meeting when there was a lot of concern over cryptogenic stroke in the setting of atrial fibrillation (AF) or patent foramen ovale (PFO), a small opening between the two atria (top chambers) of the heart. There was a huge debate on how or when to close the PFO."
That stimulating environment catalyzed the idea of starting the collaborative specialty clinic — the Heart Brain Clinic — that offers patients the focused expertise, dialogue and interaction of cardiology and neurology specialists in the same two-hour appointment in the same space. "There is no moving place to place, no waiting weeks to see another specialist," Dr. Ammash notes. "In this way, we create value by serving the patient with expert, multidisciplinary care and convenience in the same appointment."
Heart brain linkage
Dr. Ammash consulted with his cardiology colleagues and teamed up with Robert D. Brown Jr., M.D., M.P.H., a neurologist at Mayo Clinic's campus in Rochester to open one of the first advanced multidisciplinary heart brain clinics. As chair of the Division of Cerebrovascular Diseases in the Department of Neurology, Dr. Brown immediately saw the potential for improving patients' lives with real-time collaborative consults by teams of advanced subspecialists probing the heart-brain linkage driving stroke.
Heart disease, including AF, heart attack, heart failure and valvular disease, causes about 30% of ischemic strokes. For many patients, AF or the PFO is previously undiagnosed. Says Dr. Brown: "Given that about 20% to 25% of the population has a PFO, it can be difficult to know with certainty if the PFO is the cause of the stroke or TIA. In addition, the decision regarding the best management approach for PFO, atrial fibrillation and other cardiac conditions in the setting of a stroke or TIA can be complex, leading to the importance of a Heart Brain Clinic type of approach, allowing joint decision-making with a neurologist, a cardiologist and the patient."
Success drives expansion
To meet patient demand, the Rochester campus has increased Heart Brain Clinic consults to two half-days a week — up from once a week. There is also a Heart Brain Clinic at Mayo's campus in Jacksonville, Florida. In the year since it opened, this clinic, too, has flourished, and to meet demand, Heart Brain Clinic consults take place every other week, up from once a month.
Explains Michelle P. Lin, M.D., M.P.H., a neurologist and the co-director of the Heart Brain Clinic on Mayo's Florida campus: "There is a real and urgent need for this kind of care. In the U.S., cryptogenic stroke accounts for 20% to 30% of all ischemic strokes, translating to approximately 160,000 to 240,000 U.S. patients annually. The condition is especially common in young patients who have no other identifiable symptoms or risk factors for stroke. With two multidisciplinary providers caring for each patient, the likelihood of getting the right diagnoses increases."
"Undiagnosed AF or PFO are both common triggers for many stroke patients. The collaborative nature of the Heart Brain Clinic allows us to determine whether patients with heart disease will benefit from surgery or medical treatment to prevent stroke or hemorrhage," she explains.
Target populations
In their evaluations, Dr. Lin and colleagues currently target patients in two main cardiac populations to determine if they would benefit from minimally invasive closure procedures to reduce the risk of stroke:
- Patients with atrial fibrillation with bleeding or fall risks who cannot tolerate long-term anticoagulation for ischemic stroke prevention. These patients tend to be an older population.
- Patients with PFO who have had TIA or stroke. These patients tend to be a younger population.
Explains her colleague Peter M. Pollak, M.D., an interventional cardiologist at Mayo Clinic's Florida campus and co-director of the Heart Brain Clinic there: "Because patients are seen by a cardiologist and a neurologist in the same visit, we can efficiently determine and communicate the best evaluation and treatment plan to prevent further events and complications."
Pathological ambiguity of PFO
Nearly 2 billion people around the world are affected by PFO from birth, according to Dr. Pollak. This means that for about 1 in 4 people, the flap between the right atrium and left atrium does not seal properly.
Yet many people may never know they have a PFO and may not experience ill effects. This pathological ambiguity makes it difficult for nonspecialists to know how to manage PFO — or makes them prone to managing it unnecessarily, exposing patients to extra risks and costs.
Says Dr. Pollak: "If you've had a stroke and you're found to have a PFO, it is really important to see a collaborative clinic with a neurologist and a cardiologist to figure out whether closing your PFO will reduce the likelihood of recurrent stroke or another event."
AF and the left atrial appendage
The Heart Brain Clinic also sees many patients diagnosed with AF. Because this heart rhythm disorder — characterized by irregular, chaotic beating — decreases the heart's blood-pumping efficiency, it also increases a patient's risk of stroke. The risk typically arises from clots that may form in the left atrial appendage. Lifelong treatment with warfarin blood-thinning therapy or a direct oral anticoagulant is typically effective in preventing clot formation that leads to stroke.
However, some people cannot tolerate blood thinners. Or they have other issues that may lead doctors to recommend implanting a small device, called the Watchman device, to close the left atrial appendage.
Indications for the Watchman device
Dr. Ammash notes that one of the unusual specialties of Mayo's Heart Brain Clinic model is its early consideration of treatment with the Watchman device in AF patients with stroke and significant bleeding. This permanent implantable device is an alternative to lifelong anticoagulant therapy. Its goal is to reduce the risk of stroke by treating nonvalvular AF.
According to Dr. Lin, a key benefit of the Mayo Heart Brain Clinic model is the collaboration it supports in real time that leads to shared decisions individualized to each patient.
Adds Dr. Ammash: "The Heart Brain Clinic adds value. We do not close PFO unnecessarily. For me, the most important thing we do is identifying the right patient who needs a procedure and those who do not. I really want to make sure we are choosing the right patients for the procedures that have risks of stroke and other complications, not to mention costs. That's ultimately how we improve patient quality of life."