Feb. 22, 2022
The incidence of post-diversion ureteroenteric anastomotic stricture (UES) approaches 15%. "Compelling data suggests that this condition carries morbidity and adversely impacts patients' quality of life," says Boyd R. Viers, M.D., a urologist at Mayo Clinic in Rochester, Minnesota.
In a study of a series of 2,285 patients undergoing cystectomy with urinary diversion with a median 10 years of follow-up — published in Translational Andrology and Urology in 2020 — several important findings were noted:
- Benign UES tended to occur early, with 75% being diagnosed within two years of surgery.
- There was a nearly 0.5% incidence each year thereafter, highlighting the need for long-term upper tract surveillance.
- While the majority of the patients were symptomatic, 1 in 4 presented with silent obstruction.
Ultimately, patients with UES after urinary diversion are 1.6 times more likely to have progression of chronic kidney disease, as noted in a study published in The Journal of Urology in 2014.
Dr. Viers notes: "Unfortunately, multiple series have demonstrated that endoscopic management of UES is temporizing at best. Review of our institutional experience revealed that strictures greater than 1 cm in length and those diagnosed within six months of urinary diversion were associated with an abysmal 0% success rate with endoscopic treatment. Rapid occurrence of complex strictures after diversion likely reflects an ischemic insult with a high probability of scar re-formation and injury progression following dilation or incisional techniques. Longitudinal endoscopic patency rates at one, two and three years were 15%, 15% and 5%, respectively, as reported in research published in Urology in 2001.
A role for definitive reconstruction in this patient population?
Revisión intraoperatoria de anastomosis uretero-entérica
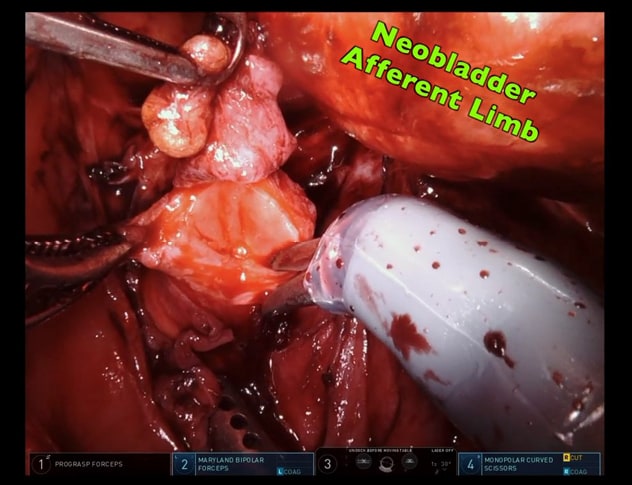
Revisión intraoperatoria de anastomosis uretero-entérica
La imagen muestra la revisión intraoperatoria de una anastomosis urétero-entérica en un paciente con neovejiga.
Research published in Urologic Oncology in 2017 confirmed that several high-volume institutions have demonstrated that open ureteral reconstruction after urinary diversion is challenging and associated with significant postoperative morbidity, including major complications in up to 20% and lengthy post-surgical hospitalization (median six days). As such, formal UES reconstruction has been reserved only for patients who fail conservative therapies such as long-term nephroureteral stents.
Advantages of the robotic platform are well suited to address some limitations of open ureteral reconstruction. These advantages include magnified visualization and instrument dexterity, near infrared fluorescence imaging to assess tissue perfusion and enable ureteral identification, and dual-inset imaging.
A contemporary analysis of 30-day morbidity associated with ureteral reconstructive procedures (open versus minimally invasive) in a national database demonstrated that an open approach was associated with increased 30-day morbidity across multiple postoperative outcome measures. The study was published in Journal of Endourology in 2021.
Dr. Viers concludes: "Undoubtedly there is an element of selection and reporting bias in recent studies. Nevertheless there has been increasing adoption of minimally invasive robotic techniques for upper tract ureteral reconstruction.
"Selective deployment of the robotic platform is critical to ensure safe and effective ureteral reconstructive outcomes. Said another way, a robotic approach may not be appropriate for all patients. In the case of robotic reconstruction of UES, several unique features warrant discussion.
"In all cases, removal of nephroureteral stent, ureteral rest and precise stricture staging are essential to ensure reconstructive success. Open series have found that UES reconstruction in the setting of indwelling nephroureteral stents was associated with a 10-fold greater risk of failure.
"As in urethral reconstruction, it is also important to characterize previous UES endoscopic treatments, as these are associated with greater blood loss and reconstructive operative time, reflecting a higher degree of complexity due to surrounding tissue fibrosis from urinary extravasation.
"Intraoperatively, synchronous antegrade ureteroscopy is beneficial to facilitate efficient ureteral identification and precise stricture localization. Intravascular indocyanine green is reserved for tissue perfusion assessment to ensure a well-vascularized, tension-free repair.
"Lastly, end-organ vascular perfusion of ureters in the setting of urinary diversion is tenuous, and therefore, avoidance of excessive manipulation and circumferential dissection (which also avoids risk of major vascular injury) should be considered when feasible.
"To date, in carefully selected patients with the adoption of these reconstructive principles, we have been able to achieve safe and durable robot-assisted UES reconstructive outcomes, including markedly reduced major complications (6%), shortened length of hospitalization (median two days) and equivalent reconstructive success. Ultimately, regardless of the tools used in the setting of advanced upper tract reconstruction, we must be prepared to climb the reconstructive ladder and selectively employ techniques that will enable a well-vascularized, widely patent and tension-free reconstruction."
For more information
Yang DY, et al. Persistent, long-term risk for ureteroenteric anastomotic stricture formation: The case for long term follow-up. Translational Andrology and Urology. 2020;9:142.
Eisenberg MS, et al. Long-term renal function outcomes after radical cystectomy. The Journal of Urology. 2014;191:619.
DiMarco DS, et al. Long-term results of treatment for ureteroenteric strictures. Urology. 2001;58:909.
Packiam VT, et al. Lessons from 151 ureteral reimplantations for postcystectomy ureteroenteric strictures: A single-center experience over a decade. Urologic Oncology. 2017;35:112e19.
Herbert KJ, et al. Contemporary analysis of ureteral reconstruction 30-day morbidity utilizing the National Surgical Quality Improvement Program (NSQIP) database: Comparison of minimally invasive versus open approaches. Journal of Endourology. 2021. In press.
Refer a patient to Mayo Clinic.