Aug. 29, 2023
Mario Hevesi, M.D., Ph.D., an orthopedic surgeon and sports medicine specialist at Mayo Clinic in Rochester, Minnesota, is passionate about improving the lives of patients diagnosed with patellofemoral instability, a complex, often undertreated knee condition. This condition comprises approximately 3% to 4% of all knee presentations to medical professionals.
"Due to its relative rarity, patellofemoral instability isn't seen by many healthcare professionals, but it's important to keep in mind as you see patients with knee symptoms, particularly given the variety of underlying factors involved," says Dr. Hevesi.
Treatment challenges for this patient population
Dr. Hevesi describes patellofemoral instability as often considered challenging to treat, especially since few patients present with only one risk factor for the condition. Patients usually experience one or more patellar (kneecap) dislocation events, usually lateral in nature.
Previously described factors that increase the risk of patellofemoral instability include:
- Patella alta. This involves a high-riding patella that can miss the trochlear groove, which is intended to keep the patella "on track" in deeper knee flexion.
- Genu valgum. This condition, also commonly known as knock-knee, may cause one or more of the knees to turn inward, resulting in the patella riding laterally toward the outside of the knee.
- Increased tibial tuberosity-trochlear groove (TT-TG) distance. This measurement between the tibial tubercle (place where the patellar tendon meets the bone) and the trochlear groove (the track in the femur for the patella) is a marker of how straight or curved the path is for the kneecap between the inner (medial) and outer (lateral) aspect of the knee. In a study in a 2019 issue of Clinical Orthopaedics and Related Research, Dr. Vairo and colleagues found that patients whose TT-TG was increased tended to have increased rates of instability.
Nearly all patients who have experienced a patellofemoral instability event have at least one risk factor for a repeat dislocation. This may be in the form of the above-presented factors or others such as dysplasia, hyperlaxity or even young age. At the same time, many "normal" people who will never have a dislocation also demonstrate the presence of such risk factors. This means that surgical decision-making often is nuanced, choosing which factors are important to address at the time of surgery and which factors can be carefully evaluated but left alone in an informed manner.
Patients with patellofemoral instability commonly are in their early teens, but instability can arise in patients of any age. These patients often have difficulty maintaining quality of life prior to patellar stabilization, mostly due to feeling as though a dark cloud — apprehension of a potential repeat knee injury — is following them throughout their everyday lives, according to Dr. Hevesi.
"Patellar instability spans a wide spectrum," he says. "Some patients have instability events every few years; others have developmental factors that have led to obligate flexion dislocation. This means every time they bend their knees, their patellas dislocate. One patient I've treated experienced multiple dislocations at night in bed. Many of these patients are anxious or apprehensive because they don't know when their next dislocations might occur. We have the potential opportunity to substantially improve their lives and function."
Surgical repair for patellofemoral instability and referrals
 Inestabilidad femororrotuliana
Inestabilidad femororrotuliana
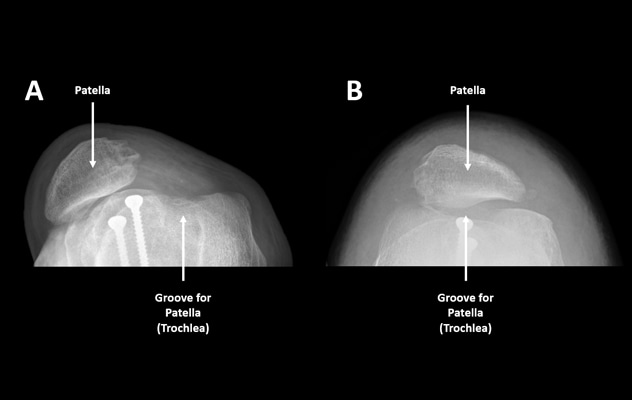
Paciente antes (A) y después (B) de la cirugía de estabilización rotuliana. Observa cómo la rótula se alinea con el surco troclear después de la reconstrucción del ligamento femororrotuliano medial y la realineación de los tejidos blandos.
Nonsurgical treatment options such as physical therapy may successfully treat some people with patellofemoral instability. However, Dr. Hevesi notes that in many instances, surgery involving restoration of the normal soft tissue restraints or "guides" of the patella, such as medial patellofemoral ligament (MPFL) reconstruction, are crucial to achieving and maintaining patellofemoral stability.
"Especially if a patient has had more than one or two dislocations and then comes to Mayo Clinic, there is a high likelihood the patient will have surgery," he says.
Surgical treatment for this condition usually involves reconstruction of the MPFL, which can be thought of as a soft tissue "seatbelt" that guides the patella into the trochlear groove of the femur. For patients with complex underlying anatomy, treatment also may include trochleoplasty, which is a reshaping of the trochlear groove, or an osteotomy, which is a realignment, of the femur or tibia.
Another procedure used for many patients with patellofemoral instability is cartilage restoration. At times, a patient's cartilage is sheared at the time of a patellar dislocation. This can lead to the cartilage becoming a loose piece within the knee, causing mechanical catching, and potentially floating to the back of the knee near important nerves, arteries and veins. The need to retrieve and repair cartilage that has found its way to the back of the knee may fall outside the scope of practice for many surgeons, according to Dr. Hevesi.
"Most surgeons who operate in the back of the knee have regular experience doing this safely and efficiently," he says. "It can be more challenging to access this area, and it's near important anatomical structures that may be at risk."
At the time of surgery, surgeons may elect to remove the floating cartilage, and if the misplaced cartilage is sizable, the surgeon may suture or otherwise screw it back in place. If the cartilage piece is small, the surgeon may send it to a lab as a biopsy. In this way, the cartilage can be grown and used in the future if needed due to ongoing symptoms or cartilage loss in a weight-bearing location important for knee function.
If the patient has been diagnosed with genu varum — also called bowleg— or genu valgum, Dr. Hevesi and colleagues may simultaneously address those underlying conditions.
In some cases of patellofemoral instability, however, Mayo Clinic orthopedic surgeons determine from the patient's medical records sent for review that their team is unlikely to add value to the treatment the patient has already received. Dr. Hevesi notes that he wants a trip to Mayo Clinic to be worthwhile for the patient. Thus, Mayo Clinic surgeons review records sent by referring healthcare professionals to try to evaluate patients pre-visit and maximize potential benefit for patients who travel to be seen.
"Whether a patient is treated in the local community or referred, we just want to be certain that something is being done to address the patient's needs," he says.
His estimate is that physicians refer approximately half of all patients diagnosed with patellofemoral instability to a tertiary or quaternary referral center. He suggests referral for surgeons who do not perform high-volume patellofemoral instability surgery.
"It's important that you get the correct positioning of the MPFL and that you take all the potential underlying factors into consideration," he says. "You're more likely to get it right if you do it often."
Dr. Hevesi also performs revision surgery for patellofemoral instability repair operations completed at other hospitals that may have failed postsurgically. He indicates that some patients on whom he operates have experienced multiple previous surgeries to remedy patellofemoral instability.
For more information
Vairo GL, et al. Tibial tubercle-trochlear groove distance is a reliable and accurate indicator of patellofemoral instability. Clinical Orthopaedics and Related Research. 2019;477:1450.
Refer a patient to Mayo Clinic.