Dec. 17, 2020
Pelvic exenteration (PE) is known to be a radical surgery, yet it's performed for the purpose of severe pain relief, life extension or even cure for patients who've experienced recurrent or persistent pelvic cancers. While offering hope for patients with otherwise poor prognosis, this radical surgery is associated with morbidity that must be balanced with benefit to the patient, including the possibility of cure.
Major complication rates with PE make candidate selection crucial, says Amanika Kumar, M.D., gynecologic surgeon at Mayo Clinic's campus in Rochester, Minnesota. Dr. Kumar and colleagues conducted a study looking at how physicians might predict potential complications in their patients and published results in Gynecologic Oncology in 2019.
Investigators' study rationale
Dr. Kumar and colleagues noted selection criteria for this extensive surgery — removing most pelvic organs, including bladder, ovaries, uterus, vagina, rectum and the lower colon — were not well defined and literature on this topic was scant. Thus, they pursued a study of pre-surgical major complication predictors, focusing on the 30 days after PE.
"We conducted this study to better understand the risk associated with this procedure," says Dr. Kumar. "Also imperative to our research team was to support providers as they counsel patients about PE."
Study design and findings
Resección en exenteración anterior
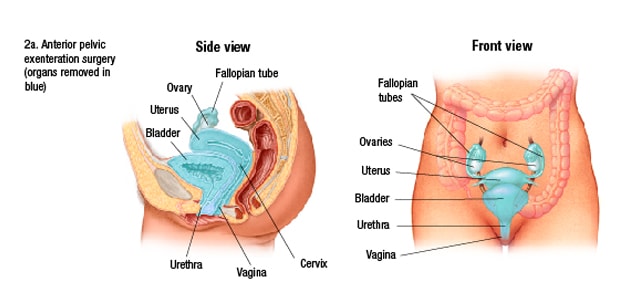
Resección en exenteración anterior
Ilustración de una resección en exenteración anterior, incluida la extirpación de la vejiga y de todos los órganos ginecológicos, lo que requiere la creación de una urostomía.
Resección en exenteración posterior
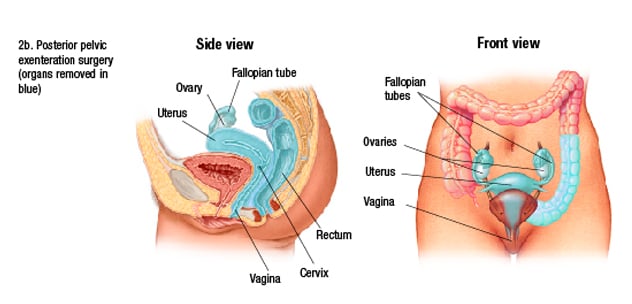
Resección en exenteración posterior
Ilustración de una resección en exenteración posterior, incluida la extirpación del recto y de todos los órganos ginecológicos, lo que requiere una colostomía permanente.
Resección en exenteración total
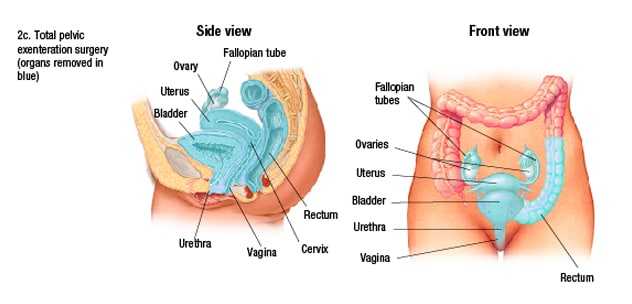
Resección en exenteración total
Ilustración de la resección en exenteración total, incluida la extirpación de todos los órganos pélvicos, lo que requiere una bolsa permanente para la orina y otra para las heces.
The investigators conducted a review study, examining patient demographics and surgical characteristics of Mayo Clinic PEs from 2004 through 2016. They utilized the Accordion Severity Grading System to evaluate postsurgical complications for 30 days after PE.
The study cohort included 138 females. Of those, 45 underwent total PE, 41 had posterior PE, and 52 underwent anterior PE. The group included patients who'd experienced cervical, endometrial, vaginal and vulvar cancers; ovarian cancer was excluded. Some study group patients had experienced gynecologic cancer treatment complications. Of the cohort, 137 underwent follow-up, with 37 women (27%) experiencing a severe post-surgical complication, and three patients (2.2%) dying within 90 days post-surgery.
Overall, the study determined 67% of women undergoing this surgery have complications within 30 days; 27% experience severe complications. After 30 days, post-surgical mortality was 0.7%, and 2.2% at 90 days. The most frequently reported complications across the board included organ system failure, infection, wound dehiscence and complications related to urinary reconstruction. The most common grade 3 complications were complications of urinary reconstruction, wound dehiscence and abdominal abscess needing intervention.
Independent predictors of severe complications post-surgically included extent of PE, especially total or anterior PE, pre-surgical hemoglobin less than or equal to 10 g/dl, and three or more comorbidities.
Additionally, patients with body mass index measurements greater than or equal to 35 or those treated with external beam radiation therapy — with or without brachytherapy — experienced more complications.
Factors Dr. Kumar and colleagues didn't find significantly associated with increased complications include abdominal surgery history, smoking, older age, American Society of Anesthesiologists score greater than or equal to 3, and preoperative albumin and creatinine levels. Also, they discovered that the primary cancer and surgical timing — whether primary or recurrent or persistent cancer treatment — had no significant bearing on severe complications.
The key postoperative complication predictor in the first 30 days is surgical complexity, Dr. Kumar's team found. Notably, they observed an elevated complication rate for surgeries involving urinary conduits. Increased complications experienced by patients with three or more comorbidities underline the importance of the patient's general health status as the surgeon and patient consider the option of PE, says Dr. Kumar.
Why PE when complications are common?
Some providers may wonder why patients undergo pelvic exenteration, given to its high complication rates. Dr. Kumar has a response. She explains: "The benefit of PE is that it can be a lifesaver for patients suffering from pain, and sometimes we can actually cure a recurrent cancer. You really can't cure a recurrent cancer anymore — as an oncologist, that's never the promise, but rather to ease suffering and complications, and maximize benefit — but with exenteration, we can sometimes offer cure.
"When cure is possible, many patients are eager to proceed with such a surgery, and we support them through their complicated recovery, teaming with our supportive care teams here and locally," says Dr. Kumar. "Complications are common, as are readmissions. But with the type of multidisciplinary care we have at Mayo Clinic, those complications are manageable."
Dr. Kumar explains that Gynecologic Oncology at Mayo Clinic's campus in Rochester, Minnesota, is nationally recognized for its work to improve perioperative care including enhanced recovery after surgery protocols, transfusion protocols, and reduction in surgical site infection projects, perioperative opioid reduction and anastomotic leak prevention. "With these efforts, we believe there is a safe way to minimize complications and improve overall patient outcomes," says Dr. Kumar.
Criteria for PE and where to have the surgery
As it may be the last opportunity for cure for patients with recurrent or persistent pelvic cancers — a population where the estimated median survival is not high — Dr. Kumar indicates there are no clear-cut pelvic exenteration exclusion criteria. Physicians can counsel patients in weighing factors such as potential quality of life, surgical complications, and life expectancy with or without PE.
Dr. Kumar advises referral to a large specialty medical center like Mayo Clinic for PE for two primary reasons: ability to bring multiple specialties to work together for the best patient outcome and higher volumes — especially experience with pelvic exenteration, which affects outcomes with the elevated surgical complexity of PE. She mentions specifically that Mayo Clinic's campus in Rochester, Minnesota, is unique in that intraoperative radiation is available with PE, a rarity in gynecologic surgery. Mayo Clinic also has a multidisciplinary team, essentially a tumor board, for gynecologic cancers.
Dr. Kumar feels passionately that pelvic exenteration should be offered to the right patients at the right medical center for this intricate surgery. "At the end of the day with cancer treatment, there's a cost to everything we do," she says. "So, helping patients understand options and treatments is imperative. We hope that with this unique care for recurrent cancer, we can offer patients an improved survival and an improved quality of life."
For more information
Tortorella L, et al. Prediction of short-term surgical complications in women undergoing pelvic exenteration for gynecological malignancies. Gynecologic Oncology. 2019;152:151.