March 24, 2023
Intracranial artery dissection (IAD) can be associated with severe clinical consequences yet have favorable outcomes when treated properly. Mayo Clinic has experience managing this rare and challenging condition.
"Intracranial dissection can present with life-threatening brain bleed, stroke or compression of critical structures of the brain. We see high numbers of patients and are actively conducting research to explore the best treatment options for this poorly understood condition," says Zafer Keser, M.D., a neurologist at Mayo Clinic in Rochester, Minnesota.
Mayo Clinic's approach includes thorough evaluations and individualized treatment recommendations from a multidisciplinary team.
Disecciones arteriales
Disecciones arteriales
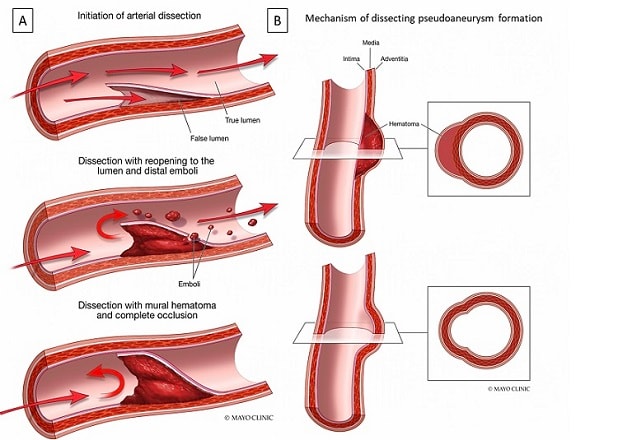
La ilustración muestra el mecanismo y la evolución de una disección arterial intracraneal (A) y de un pseudoaneurisma disecante (B).
"The pseudoaneurysms that are often present with intracranial dissections may require urgent treatment to prevent additional bleeds — hence the need for prompt involvement of an experienced vascular neurosurgeon and neurointerventionalist," says Giuseppe Lanzino, M.D., a neurosurgeon at Mayo Clinic's campus in Minnesota.
Mayo Clinic specialists have experience with endovascular and microsurgical treatment options. Asymptomatic cases can often be managed conservatively with medication and followed with repeated imaging over time.
Individuals who present with IADs are often under 60 years of age.
"The impact of IAD, unfortunately, is high. Patients can experience lifelong disabilities. When clinicians see atypical features in brain aneurysms, they should consider the possibility of IAD and refer patients to a high-volume center for further evaluation."
Team approach to diagnosis and treatment
IAD has an estimated prevalence of just 1 to 2 cases per million people. A Mayo Clinic study — published in the November 2022 issue of the Journal of Stroke and Cerebrovascular Diseases — found that the average age of individuals presenting with IAD was 57.
Asymptomatic IAD might be found incidentally on magnetic resonance (MR) angiography. "These tend to be more benign and can be managed with anticoagulants and periodic scans to monitor disease progression," Dr. Keser says. "Typically, these lesions don't rupture. The concern is clot formation in the aneurysm site that can lead to ischemic stroke."
More commonly, individuals present with a ruptured dissection or ischemic stroke. "Some people can also present with compression of neighboring structures, such as the cranial nerves," Dr. Keser says.
At Mayo Clinic, a team including vascular neurologists, vascular neurosurgeons and vascular medicine specialists evaluates each patient. Clinical genomics specialists are available if an individual has an underlying connective tissue disorder.
Vessel wall imaging is a key component of IAD evaluations. Mayo Clinic uses MR angiography, CT angiography and digital subtraction angiography to characterize the complex vascular pathologies associated with IAD. Subspecialized radiologists analyze the imaging.
"The findings can be subtle and easy for the untrained eye to miss," says Girish Bathla, M.B.B.S., M.D., a diagnostic radiologist at Mayo Clinic's campus in Minnesota. "Missing the subtle findings may lead to incorrect designation of underlying stroke etiology."
The multidisciplinary treatment team reviews options before recommending treatment. For ruptured dissections, the treatment of choice involves "trapping" the diseased vessel segment.
"This can be achieved endovascularly for intracranial dissections that are amenable to modern techniques," Dr. Lanzino says. "The development of modern stents and, more importantly, flow diverter technology allows us to reinforce and remodel the vessel lumen from within, without the need for occlusion of the involved segment."
If the vessel segment lacks sufficient collateral potential and vessel sacrifice is the best option, ligation of the involved segment and surgical bypass are indicated.
Outcomes depend on the extent of injury caused by the IAD and the potential for recurrent dissection. "Typically, recurrent events happen in the first few weeks after treatment for acute presentation. We closely monitor patients during that time for IAD recurrence or further strokes," Dr. Keser says.
Mayo Clinic's experience with IAD also facilitates post-treatment counseling for patients. "They are sometimes incorrectly told to restrict their normal daily living," Dr. Keser says. "But once these patients are past the critical post-treatment window, they can go back to normal life as long as they avoid chiropractic neck manipulation and extreme activities with a high risk of trauma."
Collaborative and translational research
Mayo Clinic is committed to translational research to improve the treatment of IAD. One research arm involves outlining the natural history and typical phenotypes of IAD.
A second effort involves documenting treatment outcomes. A study published online in Interventional Neuroradiology in 2022 reviewed the records of nearly 1,100 individuals with IAD to investigate the safety and efficacy of reconstructive and deconstructive endovascular treatment techniques.
"What we learn from our research has a direct impact on our clinical practice," Dr. Keser says. "We are sharing data with other high-volume centers internationally so that we can truly understand the predictors of recurrent dissections and other aspects of this disease."
For more information
Wahood W, et al. Trends for admissions for intracranial dissections in the United States. Journal of Stroke and Cerebrovascular Diseases. 2022;31:106723.
Essibayi MA, et al. Endovascular treatments of intracranial vertebral and internal carotid arteries dissections: An interactive systematic review and meta-analysis. Interventional Neuroradiology. In press.
Refer a patient to Mayo Clinic.